Menopause and Medical Cannabis explains how more research studies are required to establish the effectiveness and safety of medical cannabis to alleviate menopause-related symptoms.
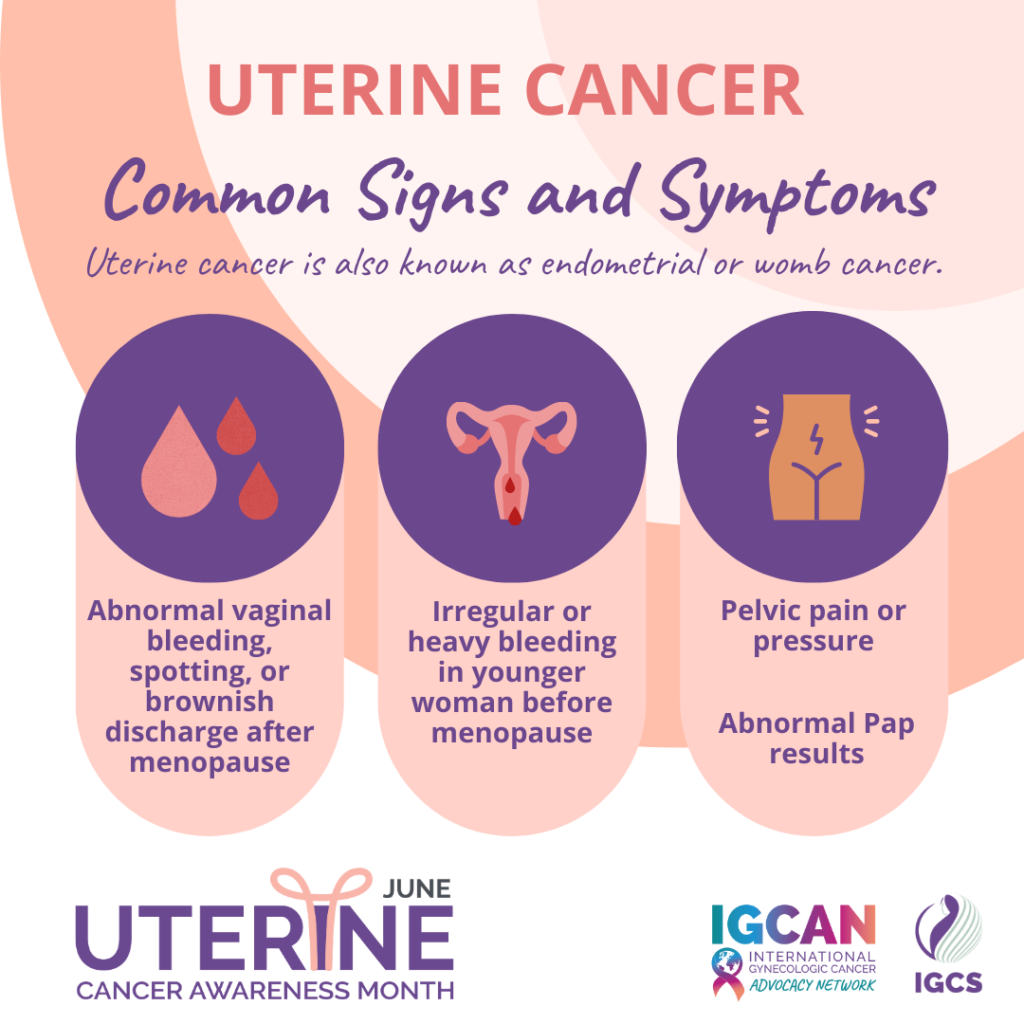
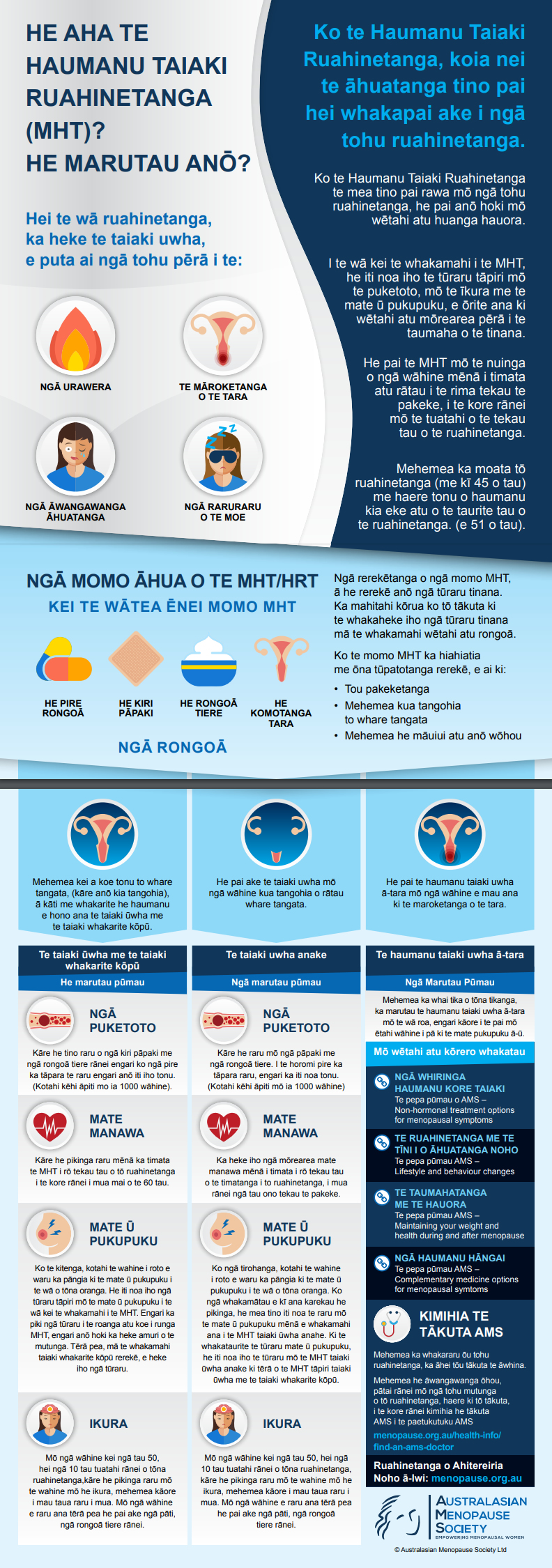
Menopause-Related Symptoms
Have studies examined the safety and efficacy of medical cannabis (MC) to alleviate menopause-related symptoms?
In More Women Turning to Medical Cannabis for Relief of Menopause Symptoms, published 03 August 2022, the North American Menopause Society note:
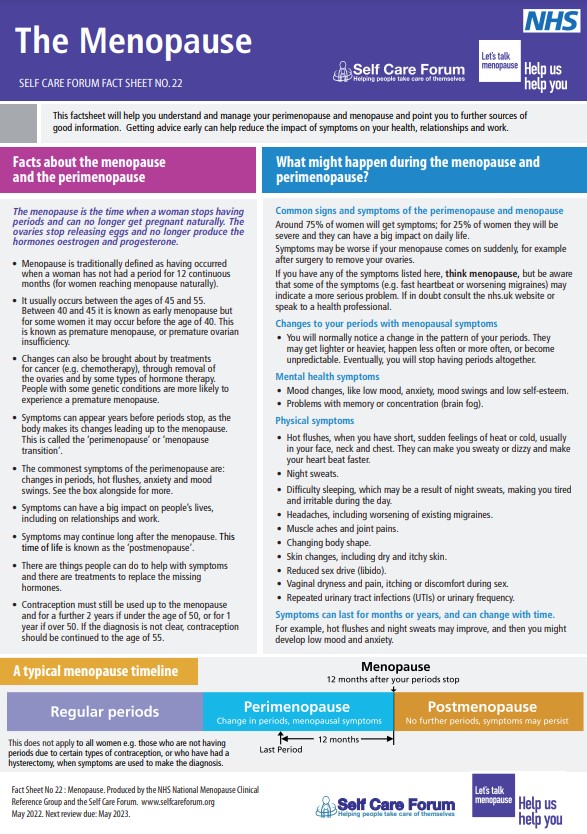
Perimenopause and Postmenopause
Did A Survey of Medical Cannabis Use During Perimenopause and Postmenopause, published 02 August 2022, examine the safety and efficacy of MC to alleviate menopause-related symptoms?
The Conclusion of the authors of A Survey of Medical Cannabis Use During Perimenopause and Postmenopause: Conclusion, with 258 participants, was:
July 2024 Study
What did the Women’s Perceptions and Experiences With Cannabis Use In Menopause: A Qualitative Study, published 09 July 2024, include in their Results?
The Results of the authors of Women’s Perceptions and Experiences With Cannabis Use In Menopause: A Qualitative Study, with 12 participants, included:
 “Women self-managed their cannabis use, learning from their own experiences or the anecdotal sharing of others’, accessed cannabis from a variety of medical and nonmedical sources, and relied on experimentation, and a range of supports were described”.
“Women self-managed their cannabis use, learning from their own experiences or the anecdotal sharing of others’, accessed cannabis from a variety of medical and nonmedical sources, and relied on experimentation, and a range of supports were described”.Healthcare Provider
What should be noted about the use of MC to relieve the symptoms of menopause?
In Cannabis May Offer Relief From Menopause Symptoms: More Research Is Needed To Understand Cannabis Use for Menopausal Symptoms the Open Access Government elaborate on:
On page two in More Women Turning To Medical Cannabis for Relief of Menopause Symptoms the NAMS note:
Health Topics A-Z
Where may I find Health Topics A-Z related to Menopause and Medical Cannabis?
In Health Topics A-Z you may find:
Links
Where may I find Links related to Menopause and Medical Cannabis?
Your Country may have Links similar to:
Links
This Links List to third party websites is neither comprehensive nor exhaustive. Inclusion on this Links List does not imply endorsement or recommendation. Non-inclusion on this Links List does not imply non-endorsement or non-recommendation. Third party websites are not under the control of Meno Martha International Menopause Directory. Third party websites may contain explicit medical images and/or sexual references. Please read Meno Martha International Menopause Directory’s Links Policy before proceeding to a Link. Please contact Webmaster if you experience a problem with a Link.New or Updated
- Cannabis Use for Menopause In Women Aged 35 and Over: A Cross-Sectional Survey on Usage Patterns and Perceptions In Alberta, Canada
- Mayo Clinic Minute: Perimenopause and Menopause [13 May 2024] [+ Video Courtesy: Mayo Clinic News Network]
- More Women Are Using Cannabis To Ease Menopause Symptoms, A Study Suggests [29 September 2023]
- Video Series-2024: Preparing for Your Menopause Healthcare Visit
- Women Are Turning To Cannabis To Treat Menopause Symptoms, Study Suggests [18 October 2023]
- Women’s Perceptions and Experiences With Cannabis Use In Menopause: A Qualitative Study [09 July 2024]
- A Survey of Medical Cannabis Use During Perimenopause and Postmenopause
- Are Women Turning To Cannabis for Menopause Symptom Relief?
- CBD Basics: What You Need To Know
- CBD Oil — Are the Benefits Claimed Too Good To Be True?
- CBD: What You Need To Know
- Cannabidiol-Treated Ovariectomized Mice Show Improved Glucose, Energy, and Bone Metabolism With A Bloom In Lactobacillus
- Cannabis May Offer Relief From Menopause Symptoms
- Cannabis Use for Menopause In Women Aged 35 and Over: A Cross-Sectional Survey on Usage Patterns and Perceptions In Alberta, Canada
- Cannabis, Menopause, and the Endocannabinoid System
- Cognitive Effects In Midlife of Long-Term Cannabis Use
- Does CBD Oil Work for Menopause Symptoms?
- Does Cannabis Actually Relieve Pain — Or Is Something Else Going On?
- Find A Menopause Practitioner [United States and Other]
- Find An AMS Doctor [Australasian Menopause Society i.e. Australia and New Zealand]
- Find Your Nearest BMS Menopause Specialist [British Menopause Society]
- Health Effects of Marijuana
- Is It Too Late To Start HRT?
- Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause
- Hot Flashes, Anxiety and Menopause: What’s the Connection?
- Hot Flashes: What Can I Do? [+ Video: What Are the Signs and Symptoms of Menopause?]
- How To Manage Menopausal Insomnia
- Later Years (Around 50 Years and Over): Menopause and Post Menopause Health – Menopause [+ Video: Menopause]
- Let’s Talk About Perimenopause
- Mayo Clinic Minute: Help With Hot Flashes Due To Menopause [+ Video Courtesy: Mayo Clinic News Network]
- Mayo Clinic Minute: Perimenopause and Menopause [+ Video]
- Medicinal Cannabis
- Medicinal Cannabis
- Medical Marijuana
- Menopause
- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Questions for Your Health Care Provider

- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Symptom Tracker

- Menopause Patient Information [Videos] 5. Lifestyle Advice In Menopause & Perimenopause
- Menopause Preparedness Toolkit Video Series: Lifestyle Tips for Menopause
- Menopause Relief In the Spotlight Thanks To Monash University-Led Studies [Australia]
- National Center for Complementary and Integrative Health: Cannabis (Marijuana) and Cannabinoids: What You Need To Know
- Navigating Menopause: Expert Insights and Solutions | Dr Susan Davis | The Proof Podcast EP 245
- Navigating Menopause: Honest Answers To All Your Questions [+ Video: What To Expect in Menopause]
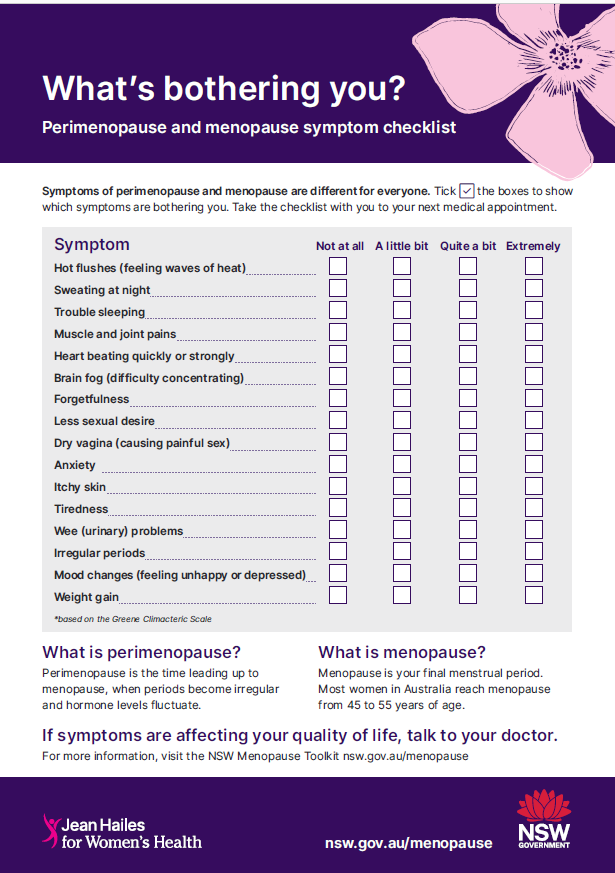
- Perimenopause and Menopause Checklist: Translated Checklists
- Perimenopause and Menopause Symptom Checklist

- Surprising Menopause Symptoms Revisited | Dr Louise Newson
- The 2023 Practitioner’s Toolkit for Managing Menopause
- The Impact of Cannabis Use on Vasomotor Symptoms, Mood, Insomnia and Sexuality In Perimenopausal and Postmenopausal Women: A Systematic Review
- Using Natural Therapies In the Menopause Transition – Webinar
- Tips To Help Manage Menopause Symptoms
- Video Series-2023: NAMS 2023 Nonhormone Therapies Position Statement for Bothersome Menopause Symptoms
- Video Series-2023: New FDA-Approved Nonhormone Option for the Treatment of Hot Flashes
- Video Series-2024: Preparing for Your Menopause Healthcare Visit
- Videos and Podcasts: Videos – How To Protect Your Brain Health At Menopause and Beyond
- Why Didn’t Anyone Tell Me This? Episode 3: Dr Annice Mukherjee: Your Essential Menopause Toolkit
- Women’s Perceptions and Experiences With Cannabis Use In Menopause: A Qualitative Study