“Before deciding on any form of treatment, talk with
your healthcare professional about your choices and
the risks and benefits of each. Review your choices yearly”.1
Umbrella
What may the Menopause Treatment Umbrella include?
Depending on the Source (DotS) this Umbrella may include:
- Menopause Medications/Medicines/Therapies/Treatments
- Menopause Symptom Medications/Medicines/Therapies/Treatments
- Menopause Therapy Choices/Options
- Menopause Treatment Choices/Options
Symptoms
How common are menopause symptoms?
On page one in the Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause, first published online 10 June 2022, one of the recommendations is:
“The use of herbs in menopause is based on longstanding traditional use, some of which is supported by scientific evidence (e.g. a recent study into the effectiveness of red clover). But more research is needed regarding the effectiveness and safety of some herbal therapies for the management of menopausal symptoms”.2
Different Differences
Is menopause treatment one-size-fits-all?
In Menopause Management Options the (Australian) Jean Hailes for Women’s Health (JH) explain:
“Many women manage mild menopausal symptoms with a healthy lifestyle. Other women with symptoms that affect their quality of life might choose to use medicines and therapies”.3
The JH also note:
 “There are many ways to manage and treat menopausal symptoms, depending on your own unique experience. You might try different options before finding a treatment that works for you. It’s important to seek accurate and reliable information before you start any treatment”.4
“There are many ways to manage and treat menopausal symptoms, depending on your own unique experience. You might try different options before finding a treatment that works for you. It’s important to seek accurate and reliable information before you start any treatment”.4 Treatments
What are some menopause treatments?
In Menopause: Diagnosis & Treatment – Treatment the (United States) Mayo Clinic elaborate on:
- Hormone Therapy…
- Vaginal Estrogen…
- Prasterone (Intrarosa)…
- Low-dose medicines to treat depression, called antidepressants…
- Gabapentin (Gralise, Neurontin)…
- Clonidine (Catapres-TTS-1, Nexiclon XR)…
- Fezolinetant (Veozah)
- Oxybutynin (Oxytrol)
- Medicines to prevent or treat the bone-thinning condition called osteoporosis…
- Ospemifene (Osphena)”.5
Hormone Therapy
How effective is hormone therapy (HT) for the treatment of hot flashes and night sweats?
On page one in Deciding About Hormone Therapy Use: Potential Benefits, published February 2025, the (United States) Menopause Society (formerly the North American Menopause Society explain:
Hormone Therapy Risks
What are the potential risks associated with HT?
On page one in Deciding About Hormone Therapy Use: Potential Risks, the Menopause Society elaborate on:
Compounded Bioidentical Hormone Therapy
Is the use of compounded bioidentical hormone therapy recommended for the treatment of menopause symptoms?
On page two in The North American Menopause Society Releases Its 2022 Hormone Therapy Position Statement, published 07 July 2022, the North American Society note:
- “Compounded bioidentical hormone therapy presents safety concerns, such as minimal government regulation and monitoring, overdosing or underdosing, presence of impurities or lack of sterility, lack of scientific efficacy and safety data, and lack of a label outlining risks”.8
On page four in the Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause one of the recommendations is:
- “The use of compounded bioidentical hormone replacement therapies is not recommended given the issues related to their purity, potency and safety. The potential benefits of bioidentical hormone therapy can be achieved using conventionally licensed products available through NHS prescribing without having to resort to compounded varieties from specialist pharmacies”.9
Healthy Lifestyle
Can a healthy lifestyle improve menopause symptoms?
On page one in the Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause one of the recommendations is:
- “Women should be advised that implementing or maintaining a healthy lifestyle can improve menopause symptoms. A healthy diet (one low in saturated fat and salt and rich in calcium and vitamin D), stopping smoking, reducing alcohol intake and including regular exercise can be beneficial. Reducing caffeine intake may also improve symptoms”.10
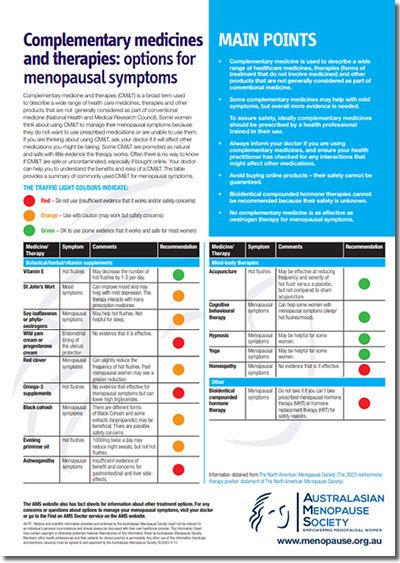
Complementary and Integrative Health
Can complementary and integrative health improve some menopause symptoms?
On page one in the Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause one of the recommendations is:
- “Alternative therapies, including cognitive behavioural therapy, may also improve hot flushes, nights sweats and other menopausal symptoms and can be considered in women who do not wish to take HRT or have contraindications to taking HRT”.11
In Menopause and Natural Therapies the JH include:
“Note that complementary and alternative medicines should be prescribed by a health practitioner trained in their use. It’s important to tell your doctor if you use these, as some herbal remedies can affect other prescribed medicines”.12
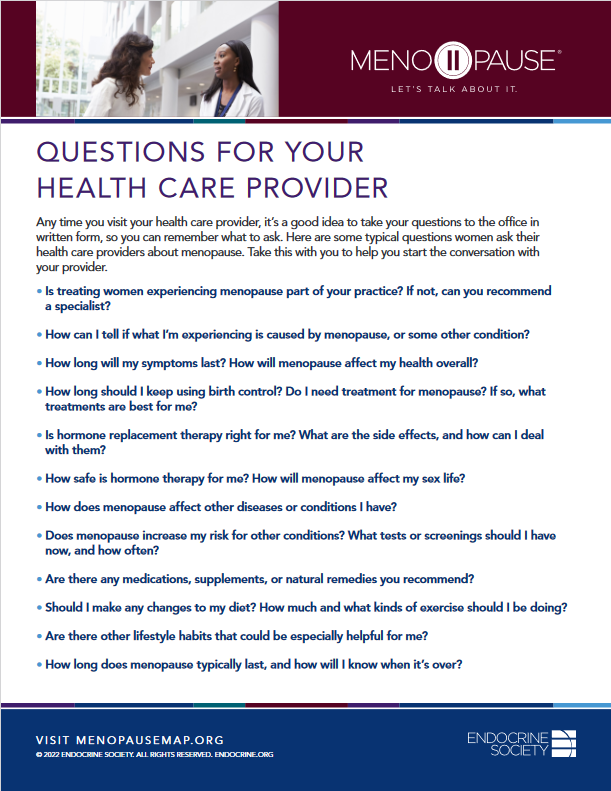
Health Care Provider
What if I would like help with menopause treatments?
If you would like help with menopause treatments, it may be in your best interest to choose to talk to your health care provider about this. The Mayo Clinic explain:
“Before deciding on any form of treatment, talk with your healthcare professional about your choices and the risks and benefits of each. Review your choices yearly. Your needs and the treatment choices may change”.13
Health Topics A-Z
Where may I find Health Topics A-Z related to Menopause Treatment?
In Health Topics A-Z you may find:
Links
Where may I find Links related to Menopause Treatment?
Your Country may have Links similar to:
Links
This Links List to third party websites is neither comprehensive nor exhaustive. Inclusion on this Links List does not imply endorsement or recommendation. Non-inclusion on this Links List does not imply non-endorsement or non-recommendation. Third party websites are not under the control of Meno Martha International Menopause Directory. Third party websites may contain explicit medical images and/or sexual references. Please read Meno Martha International Menopause Directory’s Links Policy before proceeding to a Link. Please contact Webmaster if you experience a problem with a Link.New or Updated
- Evolving Approaches To Vasomotor Symptoms In Menopause: Novel Pathways and Emerging Therapies [31 October – 16 December 2025]
- FDA Direct: Removing Black Box Warnings for HRT (Part 1/2) [10 November 2025]
- Genevieve Neal-Perry, MD, PhD, Discusses New Nonhormonal Treatments for Hot Flashes [12 December 2025]
- How Vaginal Hormones Can Transform the Health of Women [24 November 2025]
- International Menopause Society (IMS) Recommendations and Key Messages on Women’s Midlife Health and Menopause [23 December 2025]
- Navigating Menopause Care Resource Guide [03 September 2025]
- The Menopause Gap: Why Some Women Suffer More and Get Less Care [08 January 2026]
- Webinars: Lifestyle Medicine
- ACOG Explains: Managing Menopause Symptoms [American College of Obstetricians and Gynecologists]
- Askearlymenopause.org [Ask EM] [+ Video: What Is Early Menopause?]
- CAMS Menopause Hour: A Practical Approach To the Management of Menopause [Council of Affiliated Menopause Societies]
- CBT for Menopausal Symptoms
- Cognitive Behaviour Therapy (CBT) for Menopausal Symptoms
- Complementary & Alternative Therapies: Non-Hormonal Treatments for Menopause Symptoms
- Complementary Medicines and Therapies for Hot Flushes
- Complementary Medicines and Therapies: Options for Menopausal Symptoms
- Consumer Video and Podcast Series: 2023 Consumer Videos and Podcasts – NAMS 2023 Nonhormone Therapies Position Statement for Bothersome Menopause Symptoms
- Consumer Video and Podcast Series: 2024 Consumer Videos and Podcasts – Cognitive Behavioral Therapy and Menopause
- Consumer Video and Podcast Series: 2024 Consumer Videos and Podcasts – Preparing for Your Menopause Health Care Visit
- Deciding About Hormone Therapy Use
- Evolving Approaches To Vasomotor Symptoms In Menopause: Novel Pathways and Emerging Therapies [31 October – 16 December 2025]
- Experts Answer Your Menopause Questions In New Video
- FDA Direct: Removing Black Box Warnings for HRT (Part 1/2)
- FDA Direct: Removing Black Box Warnings for HRT (Part 2/2)
- Find A Menopause Practitioner [United States and Other]
- Find A Practitioner [Australasian Menopause Society i.e. Australia and New Zealand]
- Find Your Nearest BMS Menopause Specialist [British Menopause Society]
- Genevieve Neal-Perry, MD, PhD, Discusses New Nonhormonal Treatments for Hot Flashes
- Genitourinary Syndrome of Menopause
- Genitourinary Syndrome of Menopause
- HRT Questions Answered
- Handling Hot Flushes and Night Sweats| Dr Louise Newson
- Hormone Replacement Therapy (HRT)
- Hormone Therapy: Is It Right for You?
- Hot Flashes
- Hot Flashes
- Hot Flashes: What Can I Do? [+ Video: What Are the Signs and Symptoms of Menopause?]
- Hot Flushes, Night Sweats, Brain Fog? Here’s What We Know About Phytoestrogens for Menopausal Symptoms
- How To Find Relief for Hot Flashes At Night
- How To Manage Menopausal Symptoms
- How To Talk To Your Doctor About Menopause
- How Vaginal Hormones Can Transform the Health of Women
- IMS Interview Series for Women: Lifestyle Medicine With Prof. Rossella Nappi | For Women
- International Menopause Society (IMS) Recommendations and Key Messages on Women’s Midlife Health and Menopause
- Is It Too Late To Start HRT?
- Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause
- Later Years (Around 50 Years and Over): Menopause and Post Menopause Health – Signs and Symptoms [+ Video: Talking Menopause With Your GP]
- Looking After Yourself Around the Time of Menopause
- Management of Menopausal Symptoms: A Review
- Managing Menopause Symptoms [+ Video Courtesy: Mayo Clinic News Network]
- Managing Your Symptoms
- Mayo Clinic Minute: Perimenopause and Menopause [+ Video]
- Mayo Clinic Q and A: Perimenopause Transitions and Concerns
- Menopause
- Menopause
- Menopause
- Menopause
- Menopause

- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Questions for Your Health Care Provider
- Menopause Symptoms: Mayo Clinic Expert Outlines Hormone and Nonhormonal Therapies
- Menopause Treatments: What Works, What Doesn’t
- Menopause and HRT: Fact and Fiction [Video]
- Menopause and Mental Health
- Menopause Treatment Options After Cancer
- Menopause: Diagnosis & Treatment – Treatment
- Menopause: Identification and Management [NICE Guideline Published: 12 November 2015 Last Updated: 07 November 2024]

- Mood and the Menopause
- Mymenoplan.org [My Menoplan, United States]
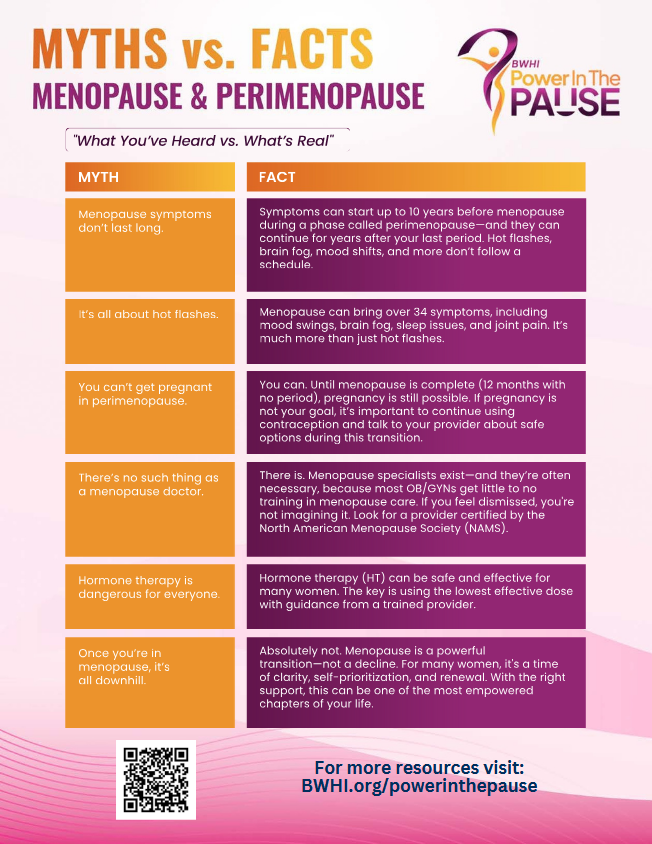
- Myth vs. Fact Menopause and Perimenopause
- National Center for Complementary and Integrative Health: Herbs At A Glance
- National Center for Complementary and Integrative Health: How Safe Is This Product or Practice?
- National Women’s Health Week [11 — 17 May 2025]: Navigating the Road to Menopause

- Navigating Menopause: Honest Answers To All Your Questions [+ Video: What To Expect in Menopause]
- Navigating Menopause Care Resource Guide
- Nonhormone Treatments for Hot Flashes and Night Sweats
- Perimenopause
- Perimenopause
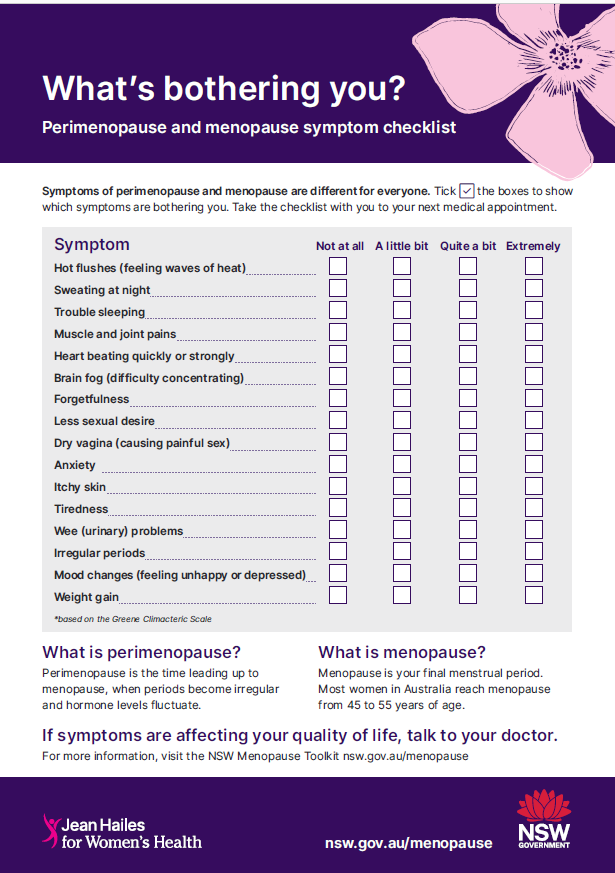
- Perimenopause and Menopause Symptom Checklist
- Q&A: What To Know When Treating Black, Hispanic and LGBTQ+ Patients During Menopause
- Resources: Fact Sheets [Multiply Languages]

- Resources: Infographics
- Resources: Posters
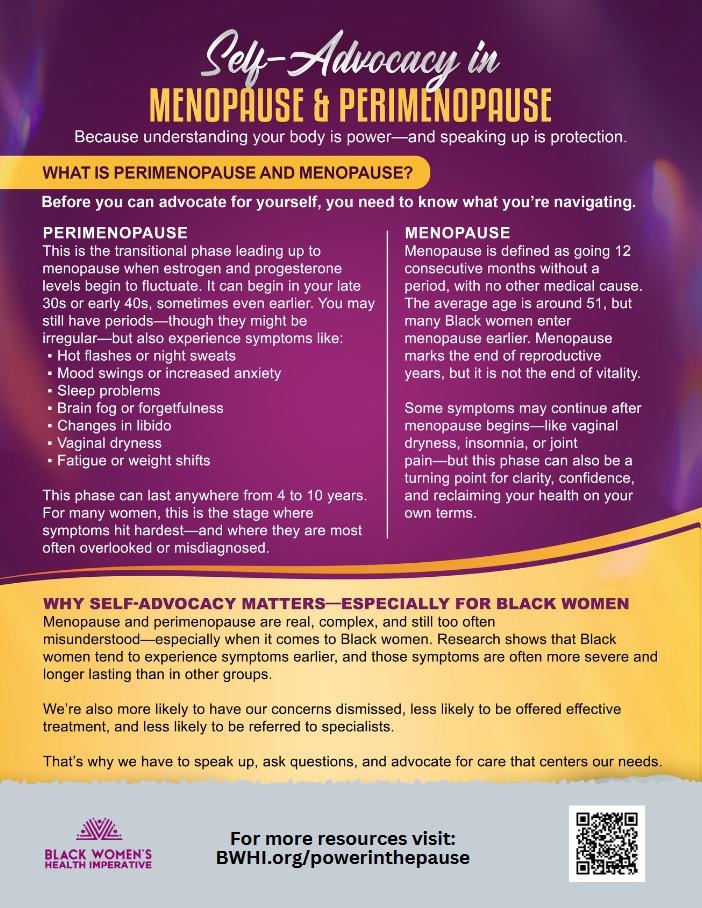
- Self-Advocacy In Perimenopause and Menopause
- Self-Help Tool: Menopause and Mental Wellbeing
- Shedding Light on the Menopause Experience and Demystifying Treatment
- Supplements: What Works, What Doesn’t and the Truth About Menowashing
- The 2023 Practitioner’s Toolkit for Managing Menopause
- The Menopause Gap: Why Some Women Suffer More and Get Less Care
- The Menopause Society Statement on Misinformation Surrounding Hormone Therapy
- The Women’s Health Initiative Randomized Trials and Clinical Practice
- Therapy Could Be Effective Treatment for Non-Physical Symptoms of Menopause
- Tips To Help Manage Menopause Symptoms
- Treatments for Menopause
- Updated 2024 NICE Menopause Guidance Summary
- Video & Podcast Library: Videos – World Menopause Day 2024: Menopause and Hormone Therapy: Current Perspectives and Controversies
- Videos & Podcasts: Videos – Menopause and Hormone Therapy: Current Perspectives and Controversies
- Webinars: Lifestyle Medicine
- Webinars: Non-Hormonal Pharmacological Interventions For VMS
- Webinars: Non-Pharmacological Interventions For VMS
- Webinars: Symposia – What’s Hot? Options for Treatment of Hot Flushes 2025
- Webinars: The Burn, the Itch, the Pain, the Urge: GSM In Women
- What if HRT isn’t right for me? And is cold-water swimming really the answer to everything? Your Menopause Questions Answered
- Why You Get An Itch or Thrush on Vaginal Estrogen and What To Do About It
- World Menopause Day 2024: Leaflet for Women – Menopause and Menopause Hormone Therapy [Multiply Languages]
- World Menopause Day 2024: Poster for Women – The 5 Ws of Menopause Hormone Therapy (MHT)
- World Menopause Day 2025
Sources
Where may I find the Sources quoted?
You may find the Sources quoted at:
Sources
- Menopause: Diagnosis & Treatment – Treatment. 07 August 2024. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/menopause/diagnosis-treatment/drc-20353401 Accessed: 11 May 2025
- Hamoda, H., Mukherjee, A., Morris, E., Baldeweg, S. E., Jayasena, C. N., Briggs, P., Moger, S. Optimising the Menopause Transition: Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause. First Published Online 10 June 2022:1 https://journals.sagepub.com/doi/10.1177/20533691221104882 Accessed: 11 May 2025
- Menopause Management Options. Last Updated: Last Updated: 24 April 2025 | Last Reviewed: 22 April 2025. Jean Hailes for Women’s Health https://jeanhailes.org.au/health-a-z/menopause/menopause-management/ Accessed: 11 May 2025
- Menopause Management Options. Last Updated: 24 April 2025 | Last Reviewed: 22 April 2025. Jean Hailes for Women’s Health https://jeanhailes.org.au/health-a-z/menopause/menopause-management/ Accessed: 11 May 2025
- Menopause: Diagnosis & Treatment – Treatment. 07 August 2024. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/menopause/diagnosis-treatment/drc-20353401 Accessed: 11 May 2025
- Deciding About Hormone Therapy Use: Potential Benefits. 2025:1. Menopause Society https://menopause.org/wp-content/uploads/default-document-library/MenoNote-Deciding-About-HT-2025.pdf Accessed: 11 May 2025
- Deciding About Hormone Therapy Use: Potential Risks. 2025:1. Menopause Society https://menopause.org/wp-content/uploads/default-document-library/MenoNote-Deciding-About-HT-2025.pdf Accessed: 11 May 2025
- The North American Menopause Society Releases Its 2022 Hormone Therapy Position Statement. 07 July 2022:2. North American Menopause Society https://menopause.org/wp-content/uploads/press-release/ht-position-statement-release.pdf Accessed: 11 May 2025
- Hamoda, H., Mukherjee, A., Morris, E., Baldeweg, S. E., Jayasena, C. N., Briggs, P., Moger, S. Optimising the Menopause Transition: Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause. First Published Online 10 June 2022:1 https://journals.sagepub.com/doi/10.1177/20533691221104882 Accessed: 11 May 2025
- Hamoda, H., Mukherjee, A., Morris, E., Baldeweg, S. E., Jayasena, C. N., Briggs, P., Moger, S. Optimising the Menopause Transition: Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause. First Published Online 10 June 2022:1 https://journals.sagepub.com/doi/10.1177/20533691221104882 Accessed: 11 May 2025
- Hamoda, H., Mukherjee, A., Morris, E., Baldeweg, S. E., Jayasena, C. N., Briggs, P., Moger, S. Optimising the Menopause Transition: Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause. First Published Online 10 June 2022:1 https://journals.sagepub.com/doi/10.1177/20533691221104882 Accessed: 11 May 2025
- Menopause and Natural Therapies. Last Updated: 07 October 2024 | Last Reviewed: 08 January 2025. Jean Hailes for Women’s Health https://www.jeanhailes.org.au/health-a-z/menopause/menopause-herbs Accessed: 11 May 2025
- Menopause: Diagnosis & Treatment – Treatment. 07 August 2024. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/menopause/diagnosis-treatment/drc-20353401 Accessed: 11 May 2025







