“Before deciding on any form of treatment, talk with
your doctor about your options and the risks and benefits
involved with each. Review your options yearly…”.1
Umbrella
What may the Menopause Physical Symptoms Umbrella include?
Depending on the Source (DotS) this Umbrella may include:
- Climacteric Changes/Symptoms
- Menopausal/Menopause Changes/Symptoms
- Menopause-Related Changes/Symptoms
- Perimenopausal/Perimenopause Changes/Symptoms
Physical Symptoms
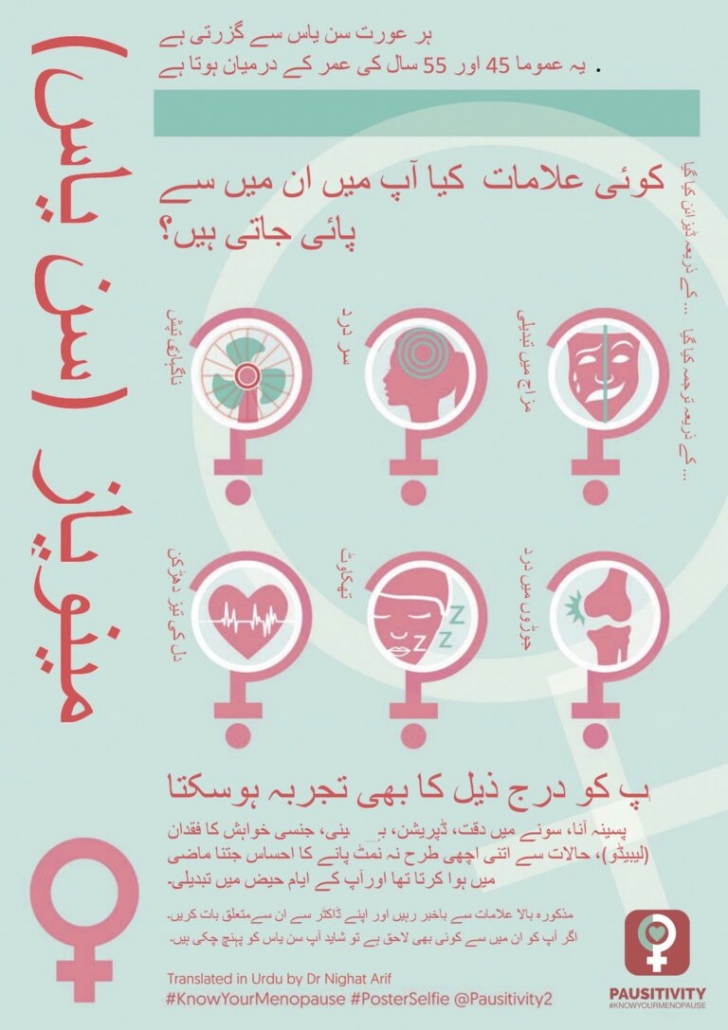
What are some menopause physical symptoms?
In Symptoms of Menopause: Physical Symptoms the (Australian) Jean Hailes for Women’s Health (JH) elaborate on:
- Irregular periods
 Hot flushes
Hot flushes- Night sweats
- Sleep problems
- Sore breasts
- Itchy, crawly or dry skin
- Exhaustion and fatigue
- Dry vagina
- Loss of sex drive (libido)
- Headaches or migraines
- More pronounced premenstrual syndrome (PMS)
- Aches and pains
- Bloating
- Urinary problems
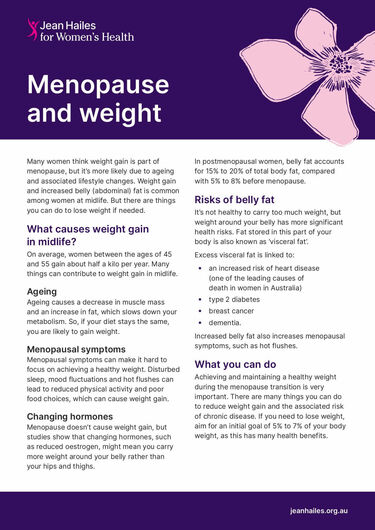
- Weight gain due to a slower metabolism”.2
Health Care Provider
What if I would like help with some menopause physical symptoms?
If you would like help with some menopause physical symptoms, it may be in your best interest to choose to talk to your health care provider about this. In Menopause: Symptoms – How Long Symptoms Last: Get Help for Symptoms the (United Kingdom) NHS note:
“Getting advice early can help reduce the impact perimenopause and menopause have on your health, relationships and work”.3
In Menopause: Diagnosis & Treatment – Treatment the (United States) Mayo Clinic explain:
“Before deciding on any form of treatment, talk with your doctor about your options and the risks and benefits involved with each. Review your options yearly, as your needs and treatment options may change”.4
Health Topics A-Z
Where may I find Health Topics A-Z related to Menopause Physical Symptoms?
In Health Topics A-Z you may find:
Links
Where may I find Links related to Menopause Physical Symptoms?
Your Country may have Links similar to:
Links
This Links List to third party websites is neither comprehensive nor exhaustive. Inclusion on this Links List does not imply endorsement or recommendation. Non-inclusion on this Links List does not imply non-endorsement or non-recommendation. Third party websites are not under the control of Meno Martha International Menopause Directory. Third party websites may contain explicit medical images and/or sexual references. Please read Meno Martha International Menopause Directory’s Links Policy before proceeding to a Link. Please contact Webmaster if you experience a problem with a Link.New or Updated
- BMS Statement on Testosterone [26 July 2024]
- How To Manage Menopausal Insomnia [04 July 2024]
- Surprising Menopause Symptoms Revisited | Dr Louise Newson [25 June 2024]
- Video Series-2024: Preparing for Your Menopause Healthcare Visit
- Videos & Podcasts: Videos – Interviews: Metabolic Syndrome in Midlife Women [April 2024]
- Webinars: Previous – Skin and Connective Tissue Ageing at the Time of the Menopause [16 July 2024]
- 5 of the Most Common Questions About Menopause
- ACOG Explains: Managing Menopause Symptoms [American College of Obstetricians and Gynecologists]
- AMS Symptom Score Card
- Askearlymenopause.org [Ask EM] [+ Video: What Is Early Menopause?]
- BMS Statement on Testosterone
- BMS TV: Bioidentical Hormones
- BMS TV: Headaches, Migraines and the Menopause
- BMS TV: Testosterone Explained
- Bioidentical Custom Compounded Hormone Therapy
- Bioidentical Hormone Therapy
- Bioidentical Hormones: Are They Safer?
- Cognitive Behaviour Therapy (CBT) for Menopausal Symptoms
- Compounded Bioidentical Hormone Therapy [Video]
- Deciding About Hormone Therapy Use
- Diagnosing Menopause
- Dr Louise Newson Breaks Down The Menopause & Lisa Snowdon Shares Her Experience | This Morning
- EMAS On-Demand Webinars [European Menopause and Andropause Society] [Multiply Languages]: Benefits of Oral Combined MHT for Estrogen Deficiency Symptoms Treatment (EN)
- Find A Menopause Practitioner [United States and Other]
- Find An AMS Doctor [Australasian Menopause Society i.e. Australia and New Zealand]
- Find Your Nearest BMS Menopause Specialist [British Menopause Society]
- HRT
- HRT – Types, Doses and Regimens
- HRT: Benefits and Risks
- Hormone Replacement Therapy
- Hormone Replacement Therapy (HRT): Alternatives To Hormone Replacement Therapy (HRT)
- Hormone Therapy: Is It Right for You?
- Hot Flashes
- Hot Flashes
- Hot Flashes, Anxiety and Menopause: What’s the Connection?
- Hot Flashes: What Can I Do? [+ Video: What Are the Signs and Symptoms of Menopause?]
- How To Manage Menopausal Insomnia
- Is Menopause Making Me Put on Weight? No, But It’s Complicated
- Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause
- Later Years (Around 50 Years and Over): Menopause and Post Menopause Health – Menopause [+ Video: Menopause]
- Later Years (Around 50 Years and Over): Menopause and Post Menopause Health – Signs and Symptoms of Menopause [+ Video: Talking Menopause With Your GP]
- Later Years (Around 50 Years and Over): Menopause and Post Menopause Health – Treating Menopause Symptoms [+ Video: Does the Menopause Happen Suddenly?]
- Let’s Talk About Perimenopause
- Looking After Yourself
- Managing Your Symptoms
- Mayo Clinic Minute: Help With Hot Flashes Due To Menopause [+ Video Courtesy: Mayo Clinic News Network]
- Mayo Clinic Minute: How Lifestyle Changes May Help Manage Menopause Symptoms [+ Video]
- Mayo Clinic Minute: Perimenopause and Menopause [+ Video Courtesy: Mayo Clinic News Network]
- Mayo Clinic Q and A: Perimenopause Transitions and Concerns
- Menopause
- Menopause
- Menopause
- Menopause
- Menopause Management Options
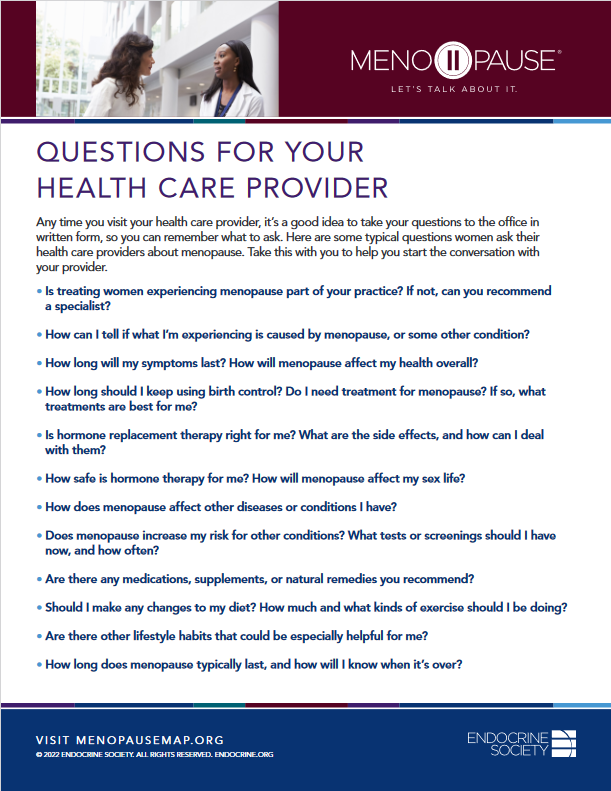
- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Questions for Your Health Care Provider

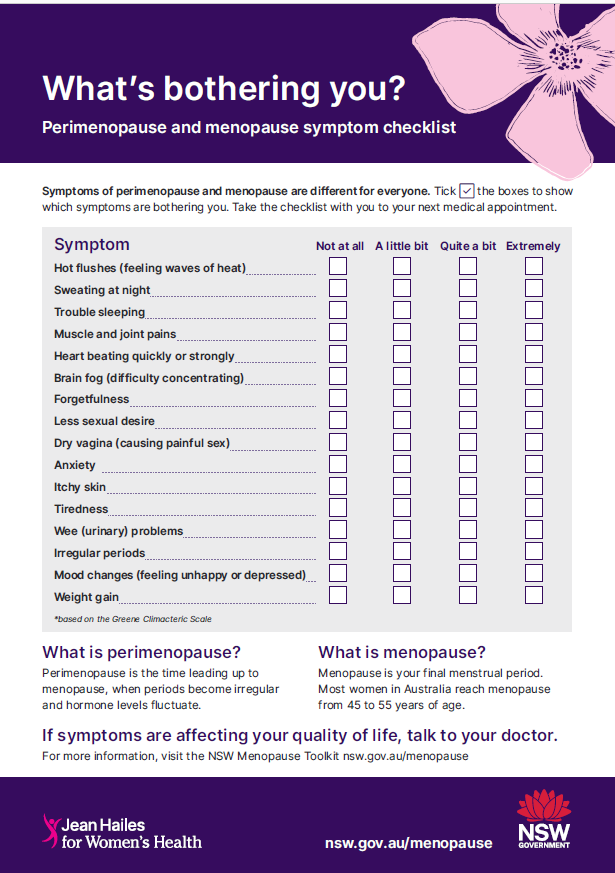
- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Symptom Tracker

- Menopause Patient Information [Videos] 1. What Is Menopause?
 Menopause Patient Information [Videos] 3. The Risks & Benefits of HRT
Menopause Patient Information [Videos] 3. The Risks & Benefits of HRT- Menopause Patient Information [Videos] 4. The Different Types of HRT
- Menopause Patient Information [Videos] 5. Lifestyle Advice In Menopause & Perimenopause
- Menopause Preparedness Toolkit: A Woman’s Empowerment Guide
- Menopause Symptoms: Mayo Clinic Expert Outlines Hormone and Nonhormonal Therapies
- Menopause Treatments: What Works, What Doesn’t
- Menopause and HRT: Fact and Fiction
- Menopause: Diagnosis and Management – Information for the Public: Questions To Ask About Menopause [NICE Guideline]
- Menopause: Symptoms
- Menopause: Symptoms & Causes
- Menopause: Understanding the Changes and Finding Relief | Dr Susan Davis | The Proof Podcast EP 256
- National Center for Complementary and Integrative Health: Herbs At A Glance
- National Center for Complementary and Integrative Health: How Safe Is This Product or Practice?
- Natural Remedies To Help Manage Perimenopause Symptoms
- Natural Therapies
- Navigating Menopause: Expert Insights and Solutions | Dr Susan Davis | The Proof Podcast EP 245
- Navigating Menopause: Honest Answers To All Your Questions [+ Video: What To Expect in Menopause]
- Night Sweats
- Non-Estrogen Treatments for Menopausal Symptoms
- Nonhormone Treatments for Hot Flashes and Night Sweats
- Perimenopause
- Perimenopause
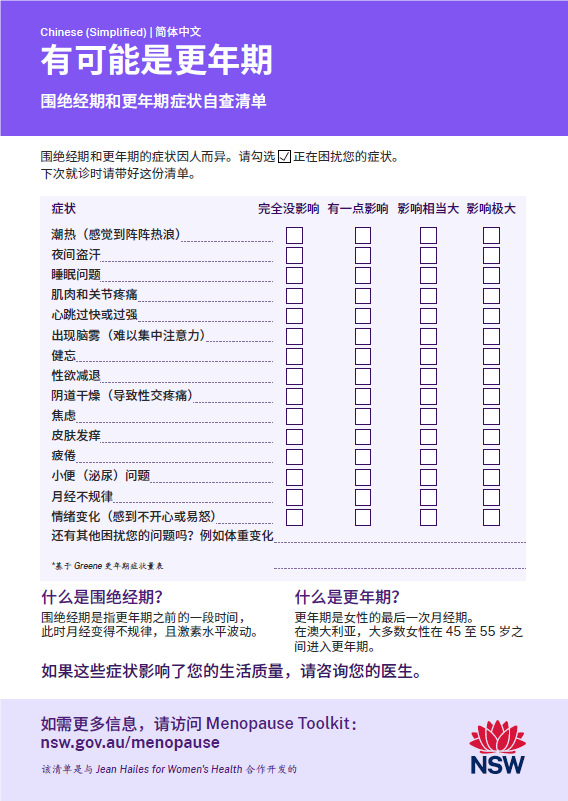
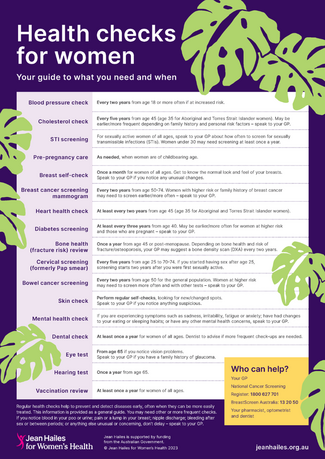
- Perimenopause and Menopause Checklist: Translated Checklists
- Perimenopause and Menopause Symptom Checklist

- Physical Activity and Exercise for Hot Flashes: Trigger or Treatment?
- Symptoms of Menopause
- Symptoms of Menopause: What Are the Symptoms of Menopause?
- The Truth About Menopause Supplements | Dr Sarah Berry
- The Women’s Health Initiative Randomized Trials and Clinical Practice
- The Women’s Health Initiative Trials: Clinical Messages
- Tips To Help Manage Menopause Symptoms
- Using Natural Therapies In the Menopause Transition – Webinar
- Vaginal Dryness
- Vaginal Dryness: What To Do About It
- Video Series-2023: NAMS 2023 Nonhormone Therapies Position Statement for Bothersome Menopause Symptoms
- Video Series-2023: New FDA-Approved Nonhormone Option for the Treatment of Hot Flashes
- Video Series-2023: Premature and Early Menopause
- Video Series-2023: Racial and Ethnic Differences In the Menopause Experience
- Video Series-2024: Preparing for Your Menopause Healthcare Visit
- Videos and Podcasts: Videos – Interviews: A Simple Approach To Menopause: The Menopause Quick Six (www.MQ6.ca)
- Videos & Podcasts: Videos – Interviews: Metabolic Syndrome In Midlife Women
- Videos & Podcasts: Videos – Interviews: Preventing Bone Loss At Menopause
- Webinars: Previous – Non-Hormonal Pharmacological Interventions For VMS
- Webinars: Previous – Non-Pharmacological Interventions For VMS
- Webinars: Previous – Skin and Connective Tissue Ageing at the Time of the Menopause
- What Doctors Wish Patients Knew About Menopause
- What Everyone Should Know About Menopause Symptoms
- Why Didn’t Anyone Tell Me This? Episode 3: Dr Annice Mukherjee: Your Essential Menopause Toolkit
- You Are Stronger Than Sarcopenia
Sources
Where may I find the Sources quoted?
You may find the Sources quoted at:
Sources
- Menopause: Diagnosis & Treatment – Treatment. 25 May 2023. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/menopause/diagnosis-treatment/drc-20353401 Accessed: 27 July 2024
- Symptoms of Menopause: Physical Symptoms. Last Updated: 21 April 2024 | Last Reviewed: 19 August 2022. Jean Hailes for Women’s Health https://jeanhailes.org.au/health-a-z/menopause/menopause-symptoms Accessed: 27 July 2024
- Menopause: Symptoms – How Long Symptoms Last: Get Help for Symptoms. Page Last Reviewed: 17 May 2022. NHS https://www.nhs.uk/conditions/menopause/symptoms/ Accessed: 27 July 2024
- Menopause: Diagnosis & Treatment – Treatment. 25 May 2023. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/menopause/diagnosis-treatment/drc-20353401 Accessed: 27 July 2024