Meno Martha’s Look for A Pattern
explains how to look for a pattern with
menopause symptoms of what’s-what-when.
Umbrella
What may the Meno Martha’s Look for A Pattern Umbrella include?
Depending on the Source (DotS) this Umbrella may include:
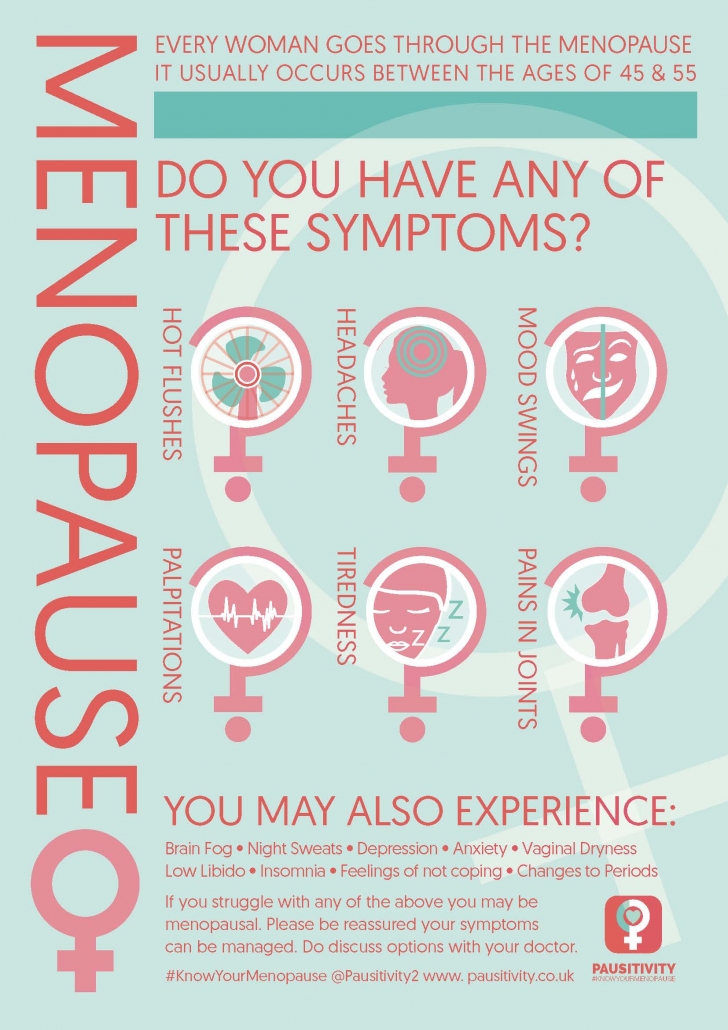
- Menopausal/Menopause Changes/Signs/Symptoms
- Menopause Transition Changes/Signs/Symptoms
- Menopause-Related Changes/Signs/Symptoms
- Perimenopausal/Perimenopause Changes/Signs/Symptoms
Menopause
What is menopause?
DotS the definition of menopause may vary. In The 2023 Practitioner’s Toolkit for Managing Menopause: Definitions, published online 01 December 2023, the authors’ definition is:
Look for A Pattern
What is the best way to predict menopause?
In What Is Menopause? Diagnosing Perimenopause and Menopause the (Australian) Jean Hailes for Women’s Health (JH) explain:
Periods Pattern
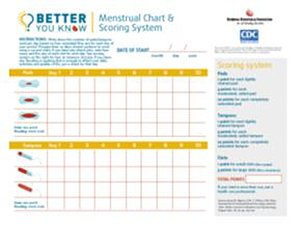
Is there a menstrual diary to look for a pattern with my periods?
Your Country may have Links similar to:
Meno Martha’s Look for A Pattern
What is Meno Martha’s Look for A Pattern?
Meno Martha’s Look for A Pattern explains how to look for a pattern with menopause symptoms of what’s-what-when.
How can I look for a pattern with my menopause symptoms?
To Look for A Pattern with menopause symptoms of what’s-what-when, you can ask yourself these questions and any of your own:
Meno Martha’s Look for A Pattern
When do you have X? e.g. When do you have hot flushes/flashes?
- Do you have X on a particular day or night of the week? e.g work day or night
- Do you have X at a particular time of day or night?
- Do you have X when you feel hot?
- Do you have X when you feel hungry?
- Do you have X when you eat spicy or certain other food?
- Do you have X when you drink tea, coffee, cola or other caffeinated drinks?
- Do you have X when you drink alcohol?
- Do you have X when you smoke?
- Do you have X when you do not have a good night’s sleep?
- Do you have X when you feel stressed or sick?
- Do you have X when you do not exercise regularly?
- Do you have X when you do something else in particular?
Meno Martha’s Look for A Flip-Side Pattern
What is Meno Martha’s Look for A Flip-Side Pattern?
Meno Martha’s Look for A Flip-Side Pattern is how to look for a pattern with menopause symptoms of what’s-what-when, you have less menopause symptoms.
 How can I look for a flip-side pattern with my menopause symptoms?
How can I look for a flip-side pattern with my menopause symptoms?
To Look for A Flip-Side Pattern with menopause symptoms of what’s-what-when, you can ask yourself these questions and any of your own:
Meno Martha’s Look for A Flip-Side Pattern
When do you have less X? e.g. When do you have less hot flushes/flashes?
- Do you have less X on a particular day or night of the week? e.g. Non-work day or night
- Do you have less X at a particular time of day or night?
- Do you have less X when you do not feel hot?
- Do you have less X when you do not feel hungry?
- Do you have less X when you eat less spicy or certain other food?
- Do you have less X when you drink less tea, coffee, cola or other caffeinated drinks?
- Do you have less X when you drink less alcohol?
- Do you have less X when you smoke less?
- Do you have less X when you have a good night’s sleep?
- Do you have less X when you do not feel stressed or sick?
- Do you have less X when you exercise regularly?
- Do you have less X when you do nothing in particular?
Hot Flush Triggers
What are hot flush triggers?
In Hot Flashes: What Can Trigger A Hot Flash the (United States) Cleveland Clinic elaborate on:
- Hot weather
- Heat
- Smoking
- Caffeine
- Alcohol
- Spicy foods
- Tight clothing
- Stress”.3
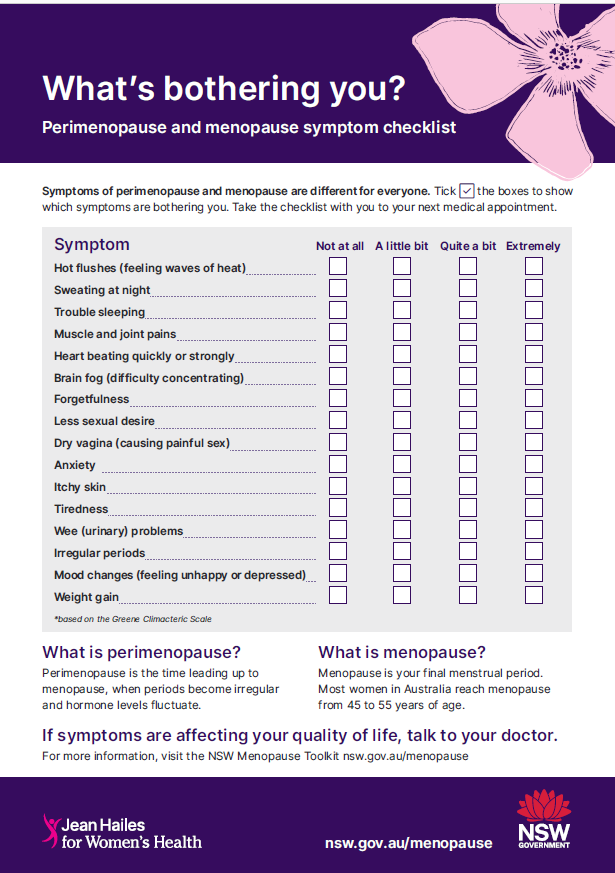
Symptom Tracker
Is there a symptom tracker?
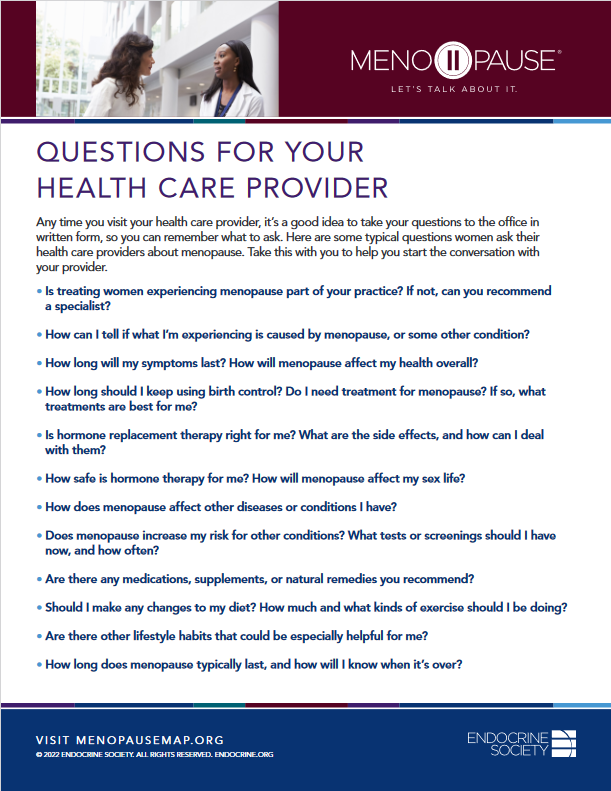
In Menopause: Related Resources – Download the Menopause Symptom Tracker the (American) Endocrine Society include:
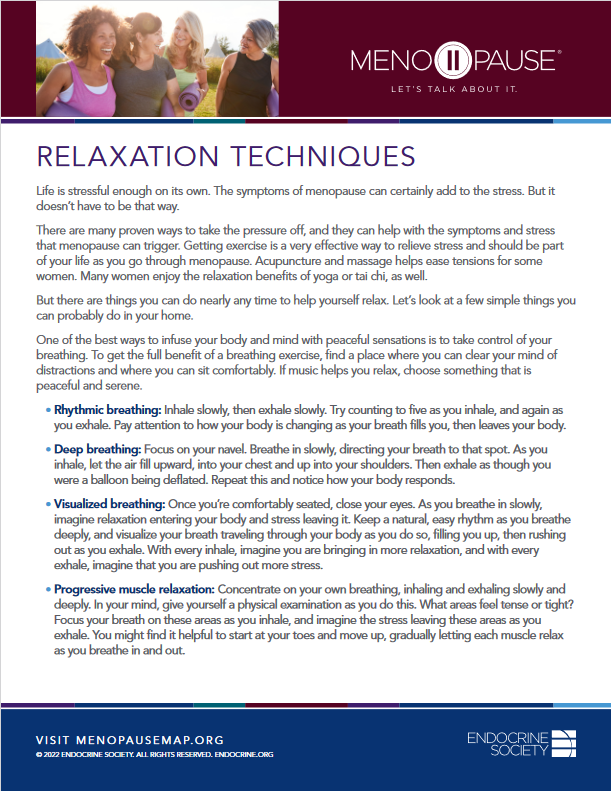
Healthy Lifestyle, Alternative Therapies, HRT
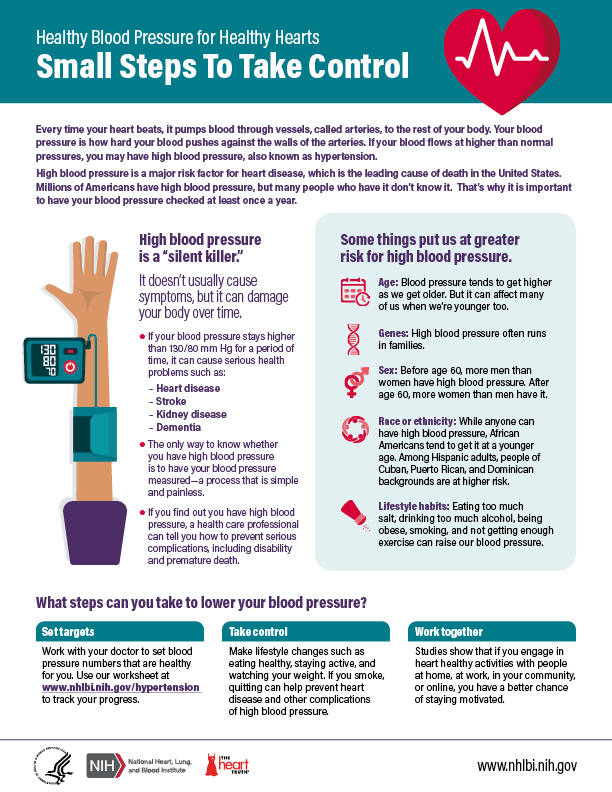
Can a healthy lifestyle, improve menopause symptoms?
On page one in the Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause, first published online 10 June 2022, the recommendations include:
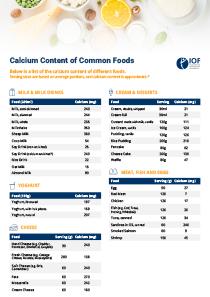
- “Women should be advised that implementing or maintaining a healthy lifestyle can improve menopause symptoms. A healthy diet (one low in saturated fat and salt and rich in calcium and vitamin D), stopping smoking, reducing alcohol intake and including regular exercise can be beneficial. Reducing caffeine intake may also improve symptoms.
- Alternative therapies, including cognitive behavioural therapy, may also improve hot flushes, nights sweats and other menopausal symptoms and can be considered in women who do not wish to take HRT or have contraindications to taking HRT.
- The decision whether to take HRT, the dose and duration of its use should be made on an individualised basis after discussing the benefits and risks with each patient…”.4
What is HRT?
HRT can be an abbreviation for Hormone Replacement Therapy.
Health Care Provider
What if I would like help with my menopause symptoms?
If you would like help with your menopause symptoms, it may be in your best interest to choose to talk to your health care provider about this.
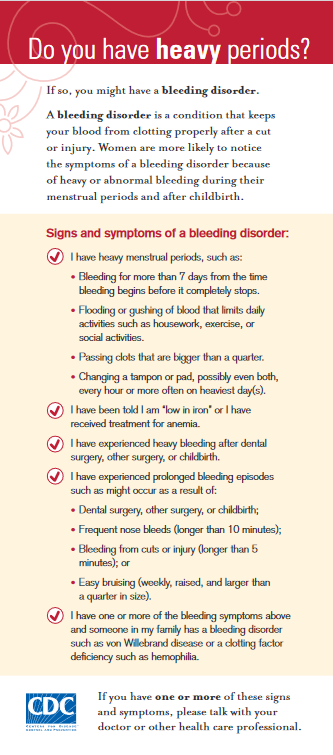
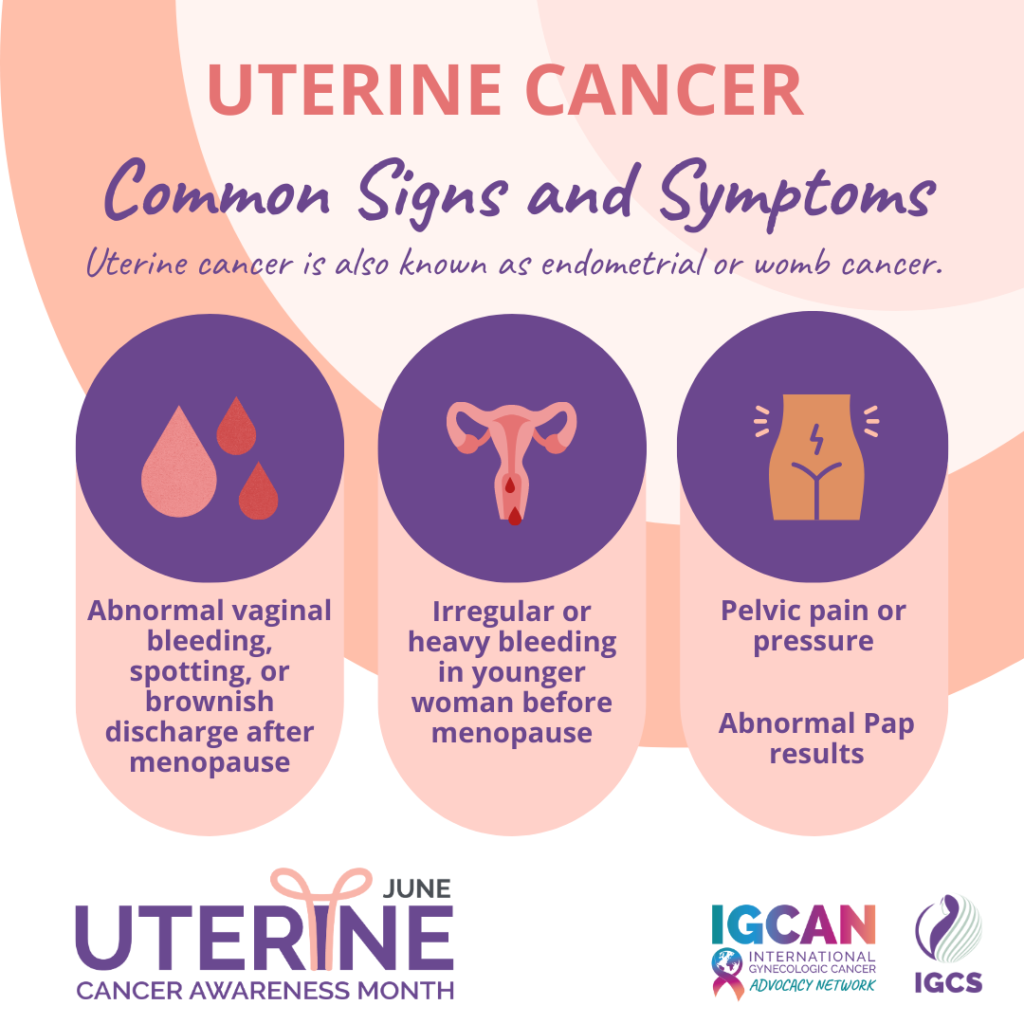
In What Is Menopause? When To See Your Doctor the JH explain:
- Irregular periods
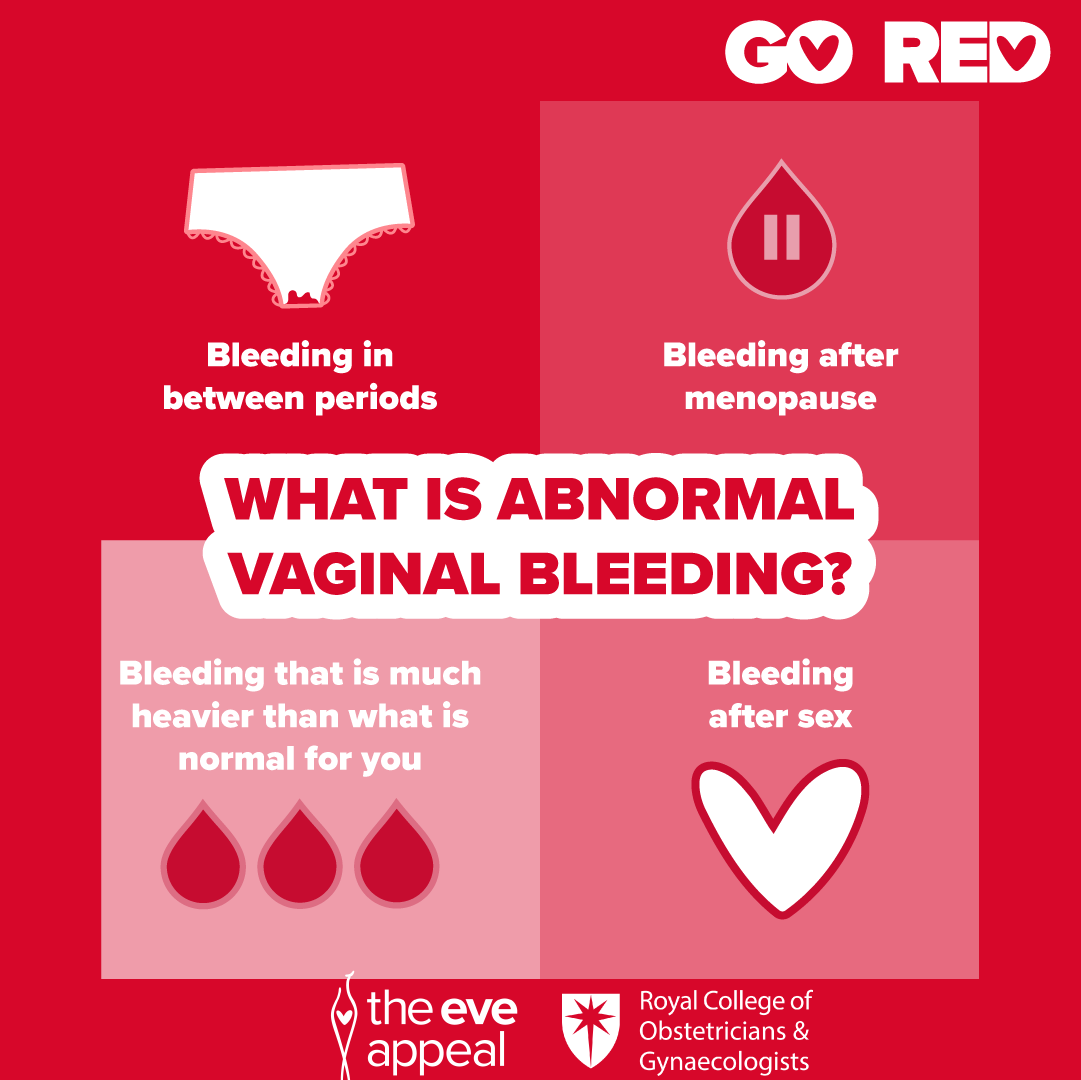
- Heavy bleeding
- Bleeding after menopause
- Increased premenstrual syndrome (PMS) symptoms
- Menopausal symptoms, such as hot flushes, that interfere with your daily life”.5
In Menopause: Diagnosis & Treatment – Treatment the (United States) Mayo Clinic also encourage us to seek help:
Health Topics A-Z
Where may I find Health Topics A-Z related to Meno Martha’s Look for A Pattern?
In Health Topics A-Z you may find:
Links
Where may I find Links related to Meno Martha’s Look for A Pattern?
Your Country may have Links similar to:
Links
This Links List to third party websites is neither comprehensive nor exhaustive. Inclusion on this Links List does not imply endorsement or recommendation. Non-inclusion on this Links List does not imply non-endorsement or non-recommendation. Third party websites are not under the control of Meno Martha International Menopause Directory. Third party websites may contain explicit medical images and/or sexual references. Please read Meno Martha International Menopause Directory’s Links Policy before proceeding to a Link. Please contact Webmaster if you experience a problem with a Link.New or Updated
- CAMS Menopause Hour – Perimenopause: A Clinical Challenge [11 March 2024]
- “Not feeling like myself” In Perimenopause — What Does It Mean? Observations From the Women Living Better Survey [25 March 2024]
- The Lancet: Series From the Lancet Journal – Menopause 2024 [05 March 2024]
- Video Series-2024: Preparing for Your Menopause Health Care Visit [13 January 2024]
- Videos & Podcasts: Videos – Interviews: Metabolic Syndrome in Midlife Women [April 2024]
- Webinars: Previous – Non-Pharmacological Interventions For VMS
- 8 Myths and Truths About Menopausal Hot Flashes
- ACOG Explains: Managing Menopause Symptoms [American College of Obstetricians and Gynecologists]
- AMS Symptom Score Card
- An Empowerment Model for Managing Menopause
- Ask Early Menopause [+ Video: What Is Early Menopause?]
- BMS TV: Menopause Explained
- Cognitive Behaviour Therapy (CBT) for Menopausal Symptoms
- Deciding About Hormone Therapy Use
- Diagnosing Menopause
- Diagnostic Tests for Menopause
- Does Having Hot Flashes Mean I’ve Started Menopause?
- Emotional Wellness In Menopause
- Find A Menopause Practitioner [United States and Other]
- Find An AMS Doctor [Australasian Menopause Society]
- Find Your Nearest BMS Menopause Specialist [British Menopause Society]
- Hot Flashes
- Hot Flashes
- Hot Flashes: What Can I Do? [+ Video: What Are the Signs and Symptoms of Menopause?]
- How Long Will I Have Hot Flashes and What Causes Them?
- How To Know If You Are In Menopause
- How To Talk To Your Doctor About Midlife Brain Fog
- I Forgot To Ask the Doctor – E9: The Menopause: Can Every Woman That Wants It Have HRT?
- Is Menopause Making Me Put on Weight? No, But It’s Complicated
- Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause
- Later Years (Around 50 Years and Over): Menopause and Post Menopause Health – Menopause [Other Languages and Formats] [+ Video: Menopause]
- Later Years (Around 50 Years and Over): Menopause and Post Menopause Health – Signs and Symptoms of Menopause [Other Languages and Formats] [+ Video: Talking Menopause With Your GP]
- Let’s Talk About Perimenopause
- Mastering Midlife Mood Changes With Marlene Freeman, MD
- Mayo Clinic Minute: Help With Hot Flashes Due To Menopause [+ Video Courtesy: Mayo Clinic News Network]
- Mayo Clinic Minute: How Lifestyle Changes May Help Manage Menopause Symptoms [+ Video]
- Mayo Clinic Q and A: Perimenopause Transitions and Concerns
- Menopause
 Menopause
Menopause- Menopause
- Menopause
- Menopause
- Menopause Checklist Podcast
- Menopause Glossary
- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Questions for Your Health Care Provider

- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Symptom Tracker
- Menopause Mindfulness: Embracing the Change of My Midlife
- Menopause Patient Information [Videos] 1. What Is Menopause?
- Menopause Patient Information [Videos] 2. Talking To Your GP About Menopause
- Menopause Patient Information [Videos] 5. Lifestyle Advice In Menopause & Perimenopause
- Menopause Preparedness Toolkit Video Series: Understanding Menstrual Health and Menopause
- Menopause Preparedness Toolkit Video Series: What Is Menopause?
 Menopause Preparedness Toolkit: A Woman’s Empowerment Guide
Menopause Preparedness Toolkit: A Woman’s Empowerment Guide- Menopause Symptoms: Mayo Clinic Expert Outlines Hormone and Nonhormonal Therapies
- Menopause Treatments: What Works, What Doesn’t
- Menopause and MS [Multiply Sclerosis]
- Menopause and Mental Health
- Menopause and Natural Therapies
- Menopause – Multiply Languages
- Menopause, Perimenopause, Hormone Therapy and Other Treatments With Madelyn Butler, MD [Podcast]
- Menopause: Definitions and Terms
- Menopause: Ensuring A Tranquil Transition
- Menopause: How Your Body Changes and What You Can Do [+ Video]
- Menopause: Is It Starting?
- Menopause: Things You Can Do
- Menstrual Calendar
- Menopause: Understanding the Changes and Finding Relief | Dr Susan Davis | The Proof Podcast EP 256
- Menstrual Diary
- Mood Changes During Perimenopause Are Real. Here’s What to Know.
- Mood and the Menopause
- My Periods Have Changed. Is Menopause Around the Corner?
- Mymenoplan.org [My Menoplan, United States]
- Navigating Menopause: Expert Insights and Solutions | Dr Susan Davis | The Proof Podcast EP 245
- Navigating Menopause: Honest Answers To All Your Questions [+ Video: What To Expect in Menopause]
- Nonhormone Treatments for Hot Flashes and Night Sweats
- Normalising Menopause
- “Not feeling like myself” In Perimenopause — What Does It Mean? Observations From the Women Living Better Survey
- Perimenopause
- Perimenopause
- Perimenopause and Menopause Checklist: Translated Checklists
- Perimenopause and Menopause Symptom Checklist

- Supporting A Loved One Through Menopause
- Symptoms of Menopause
- The Menopause
- The Reality of Menopause Weight Gain
- The Truth About Menopause Supplements | Dr Sarah Berry
- Therapy for the Effects of Menopause
- Tips To Help Manage Menopause Symptoms
- Tracking Your Cycle & Symptoms [PMS]
- Using Natural Therapies In the Menopause Transition – Webinar
- Vaginal Dryness
- Video Series-2023: NAMS 2023 Nonhormone Therapies Position Statement for Bothersome Menopause Symptoms
- Video Series-2023: Premature and Early Menopause
- Video Series-2023: Racial and Ethnic Differences in the Menopause Experience
- Video Series-2024: Preparing for Your Menopause Health Care Visit
- Videos & Podcasts: Videos – Interviews: Preventing Bone Loss At Menopause
- Videos and Podcasts: Videos – Interviews: A Simple Approach To Menopause: The Menopause Quick Six (www.MQ6.ca)
- Webinars: Previous – Non-Hormonal Pharmacological Interventions For VMS
- Whales Make Waves In the Quest To Discover Why Menopause Evolved
- What Causes Menopause?
- What Doctors Wish Patients Knew About Menopause
- What Everyone Should Know About Menopause Symptoms
- What Is Menopause?
- What Is Menopause?
- What Is Menopause? [+ Video]
- Why Didn’t Anyone Tell Me This? Episode 3: Dr Annice Mukherjee: Your Essential Menopause Toolkit
Sources
Where may I find the Sources quoted?
You may find the Sources quoted at:
Sources
- Davis, S. R., Taylor, S., Hemachandra, C., Magraith, K., Ebeling, P. R., Jane, F., and Islam, R. M. The 2023 Practitioner’s Toolkit for Managing Menopause: Definitions. Published Online: 01 December 2023 https://www.tandfonline.com/doi/full/10.1080/13697137.2023.2258783 Accessed: 21 April 2024
- What Is Menopause? Diagnosing Perimenopause and Menopause. Last Updated: 18 January 2024 | Last Reviewed: 19 August 2022. Jean Hailes for Women’s Health https://www.jeanhailes.org.au/health-a-z/menopause/about-menopause Accessed: 21 April 2024
- Hot Flashes: What Can Trigger A Hot Flash? Last Reviewed: 21 March 2022. Cleveland Clinic https://my.clevelandclinic.org/health/articles/15223-menopause-non-hormonal-treatment–relief-for-hot-flashes Accessed: 21 April 2024
- Hamoda, H., Mukherjee, A., Morris, E., Baldeweg, S. E., Jayasena, C. N., Briggs, P., Moger, S. Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause. First Published Online 10 June 2022:3-4 https://journals.sagepub.com/doi/full/10.1177/20533691221104879 Accessed: 21 April 2024
- What Is Menopause? When To See Your Doctor. Last Updated: 18 January 2024 | Last Reviewed: 19 August 2022. Jean Hailes for Women’s Health https://www.jeanhailes.org.au/health-a-z/menopause/about-menopause Accessed: 21 April 2024
- Menopause: Diagnosis & Treatment – Treatment. 25 May 2023. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/menopause/diagnosis-treatment/drc-20353401 Accessed: 21 April 2024