“The genitourinary syndrome of menopause (GSM)
includes bothersome vaginal, vulvar (lips of the vagina),
and urinary symptoms that can affect quality of life…”.1
Umbrella
What may the Genitourinary Syndrome of Menopause Umbrella include?
Depending on the Source (DotS) this Umbrella may include:
- Atrophic Vaginitis
- Genital Atrophy
- Genitourinary/Genito-Urinary Syndrome of Menopause (GSM)
- Menopause Vaginal Dryness
- Urogenital Problems
- Vaginal Atrophy
- Vaginal Dryness
- Vaginal Symptoms
- Vulvovaginal Atrophy (VVA)
Definition
What is the genitourinary syndrome of menopause (GSM)?
DotS the definition of GSM may vary. On page one in Genitourinary Syndrome of Menopause, published May 2025, the (United States) Menopause Society’s (formerly the North American Menopause Society) definition is:
“The genitourinary syndrome of menopause (GSM) includes bothersome vaginal, vulvar (lips of the vagina), and urinary symptoms that can affect quality of life, sexual satisfaction, and even your relationship with your partner. Unlike hot flashes, which typically improve with time, GSM usually worsens over time without treatment”.2
Symptoms
What may be symptoms of GSM?
In Vaginal Atrophy: Symptoms & Causes – Symptoms the (United States) Mayo Clinic explain:
- Dryness, burning or itching in the vagina
- Thin, watery, sticky, yellow or gray fluid that comes out of the vagina
- Frequent or urgent need to urinate, or a burning feeling during urination
- Losing control of the bladder, also called urinary incontinence
- More-frequent infections of the urinary tract and vagina
- Pain during sex due to less lubrication, or light bleeding after sex
- Shortening and tightening of the vaginal canal”.3
Common or Not
How common is GSM?
In Symptoms of Menopause: Bladder, Vaginal and Vulval Problems the (Australian) Jean Hailes for Women’s Health (JH) explain:
- “These symptoms are common- affecting between 40% and 90% of menopausal women. Urinary incontinence develops in up to 50% of postmenopausal women”.5
Cause
What causes GSM?
In Vaginal Atrophy: Symptoms & Causes – Causes the Mayo Clinic elaborate on:
“Genitourinary syndrome of menopause happens when the body makes less estrogen. Lower estrogen causes the tissues in the vagina to become thinner, drier, less elastic and more fragile”.6
Treatment
What are some GSM treatments?
On page one and two in Genitourinary Syndrome of Menopause the Menopause Society elaborate on:
 “There are many effective treatment options for GSM, including over-the-counter and prescription therapies. Therapies for less severe symptoms include nonhormone over-the-counter lubricants used as needed for sexual activity and moisturizers used regularly (several times per week) to maintain moisture. Prescription therapies include low-dose vaginal estrogens, vaginal dehydroepiandrosterone inserts, and oral ospemifene. Nonhormone lubricants and moisturizers can be used in combination with prescription therapies for more severe symptoms.
“There are many effective treatment options for GSM, including over-the-counter and prescription therapies. Therapies for less severe symptoms include nonhormone over-the-counter lubricants used as needed for sexual activity and moisturizers used regularly (several times per week) to maintain moisture. Prescription therapies include low-dose vaginal estrogens, vaginal dehydroepiandrosterone inserts, and oral ospemifene. Nonhormone lubricants and moisturizers can be used in combination with prescription therapies for more severe symptoms.
- “Nonhormone Remedies
- Vaginal Lubricants…
- Vaginal Moisturizers…
- Regular Sexual Stimulation…
- Expanding Your Views of Sexual Pleasure…
- Vaginal Dilators…
- Pelvic Floor Exercises…
- Vaginal Hormone Therapy…
- An effective and safe treatment, low-dose local estrogen applied directly to the vagina…
- FDA-approved low-dose vaginal estrogen products…
- Dehydroepiandrosterone (DHEA; Prasterone)
- Low-dose vaginal estrogen or DHEA may be options for women with a history breast or uterine cancer…
- Systemic Estrogen Therapy
- Other Therapies…
- Ospemifene
- Vaginal Laser Therapy…”.7
On page one in Genitourinary Syndrome of Menopause (GSM), reviewed November 2025, the British Menopause Society note:
“Whilst vaginal estrogen (also referred to as local estrogen) therapy is the best known treatment, newer drugs and interventions are now available”.8
Painful Intercourse
How may painful intercourse be resolved?
The Mayo Clinic explain:
Vaginal Estrogen
Can vaginal estrogen be placed directly into the vagina?
On page one in Deciding About Hormone Therapy Use, published February 2025, the Menopause Society explain:
“If you are bothered only by vaginal dryness, you can use very low doses of estrogen placed directly into the vagina. These low doses generally do not raise blood estrogen levels above postmenopause levels and do not treat hot flashes. You do not need to take a progestogen when using only low doses of estrogen in the vagina”.10
Prevention
How may GSM be prevented?
In Vaginal Atrophy: Symptoms & Causes – Prevention the Mayo Clinic elaborate on:
“Regular sexual activity, either with or without a partner, may help prevent genitourinary syndrome of menopause. Sexual activity increases blood flow to the vagina, which helps keep tissues in the vagina healthy”.11
Genitourinary Syndrome of Menopause: AUA/SUFU/AUGS Guideline (2025)
What is the Genitourinary Syndrome of Menopause: AUA/SUFU/AUGS Guideline (2025), published April 2025, endorsed by The International Society for the Study of Women’s Sexual Health (ISSWSH) and The Menopause Society (TMS)?
In Genitourinary Syndrome of Menopause: AUA/SUFU/AUGS Guideline (2025) the authors elaborate on:
What is AUA, SUFU and AUGS?
In the context above, these abbreviations stand for the:
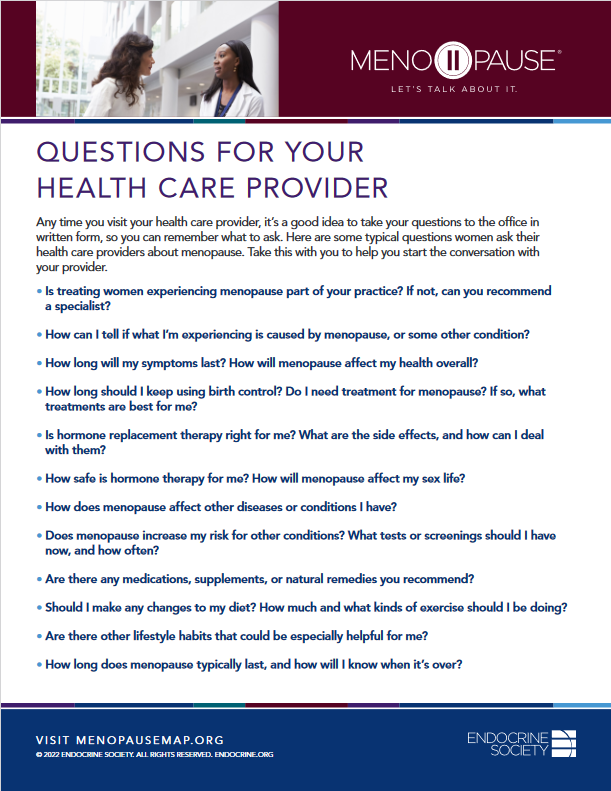
Health Care Provider
What if I think I have GSM?
If you think you have GSM it is important to talk to your health care provider. In The 2023 Practitioner’s Toolkit for Managing Menopause – Effectiveness: Local Treatment of Urogenital Atrophy, published online 01 December 2023, the authors note:
In Symptoms of Menopause: Bladder, Vaginal and Vulval Problems – Urinary Symptoms the JH explain:
Health Topics A-Z
Where may I find Health Topics A-Z related to Genitourinary Syndrome of Menopause?
In Health Topics A-Z you may find:
Links
Where may I find Links related to Genitourinary Syndrome of Menopause?
Your Country may have Links similar to:
Links
This Links List to third party websites is neither comprehensive nor exhaustive. Inclusion on this Links List does not imply endorsement or recommendation. Non-inclusion on this Links List does not imply non-endorsement or non-recommendation. Third party websites are not under the control of Meno Martha International Menopause Directory. Third party websites may contain explicit medical images and/or sexual references. Please read Meno Martha International Menopause Directory’s Links Policy before proceeding to a Link. Please contact Webmaster if you experience a problem with a Link.New or Updated
- Breast Cancer Survivors Find Relief for Debilitating Menopause Symptom [22 October 2025]
- Genitourinary Syndrome of Menopause (GSM) [November 2025]
- How Vaginal Hormones Can Transform the Health of Women [25 November 2025]
- New AUA Guideline Offers Clinicians A Practical Toolbox for GSM Management [American Urological Association] [28 November 2025]
- Use of OTC Products and Persistent Vulvovaginal Irritation In Postmenopausal Women, With Caroline Mitchell, MD, MPH [14 November 2025]
- Vaginal Laser Therapy [05 September 2025]
- Webinars: The Burn, the Itch, the Pain, the Urge: GSM In Women [15 April 2025]
- ACOG Explains: Managing Menopause Symptoms [American College of Obstetricians and Gynecologists]
- BMS TV: Urogenital Atrophy
- Bladder Control: Lifestyle Strategies Ease Problems
- Bladder Diary
- Bladder Diary
- Breast Cancer Survivors Find Relief for Debilitating Menopause Symptom
- CAMS Menopause Hour: Genitourinary Wellness In Women [Council of Affiliated Menopause Societies]
- Complementary Medicines and Therapies: Options for Menopausal Symptoms
- Complementary and Alternative Therapies for Genitourinary Syndrome of Menopause: An Evidence Map
- Consumer Video and Podcast Series: 2024 Consumer Videos and Podcasts – Preparing for Your Menopause Health Care Visit
- Deciding About Hormone Therapy Use
- Douching
- Estradiol (Vaginal Route)
- Experiencing Vaginal Dryness? Here’s What You Need To Know
- Experts Answer Your Menopause Questions In New Video
- FAQs: Vulvovaginal Health
- FDA Direct: Removing Black Box Warnings for HRT (Part 1/2)
- FDA Direct: Removing Black Box Warnings for HRT (Part 2/2)
- Find A Menopause Practitioner [United States and Other]
- Find A Practitioner [Australasian Menopause Society i.e. Australia and New Zealand]
- Find Your Nearest BMS Menopause Specialist [British Menopause Society]
- Gaslighting of Genitourinary Symptoms of the Menopause
- Genitourinary Syndrome of Menopause
- Genitourinary Syndrome of Menopause
- Genitourinary Syndrome of Menopause (GSM)
- Genitourinary Syndrome of Menopause: AUA/SUFU/AUGS Guideline (2025)
- HRT Questions Answered
- Hormonal Treatments and Vaginal Moisturizers for Genitourinary Syndrome of Menopause: A Systematic Review
- Hormone Therapy: Is It Right for You?
- Hormone Replacement Therapy (HRT): Vaginal Oestrogen – Common Questions About Vaginal Oestrogen
- Hormone Replacement Therapy (HRT): Vaginal Oestrogen – How and When To Use Vaginal Oestrogen
- Hormones and Urinary Symptoms In Women | Dr Louise Newson
- How To Talk To Your Doctor About Bladder Leakage
- How To Talk To Your Doctor About Menopause
- How To Talk To Your Doctor About Painful Sex
- How Vaginal Hormones Can Transform the Health of Women
- International Menopause Society (IMS) Recommendations and Key Messages on Women’s Midlife Health and Menopause
- International Society for the Study of Women’s Sexual Health: Find A Provider
- Is It Too Late To Start HRT?
- Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause
- Later Years (Around 50 Years and Over): Menopause and Post Menopause Health – Sexual Wellbeing, Intimacy and Menopause [+ Video: Menopause Is the End of Your Sex Life]
- Lubricant Alternatives: What To Use and What To Avoid
- Managing Menopause Symptoms [+ Video Courtesy: Mayo Clinic News Network]
- Mayo Clinic Minute: Menopause and Sexual Health [+ Video Courtesy: Mayo Clinic News Network]
- Mayo Clinic Q and A: Perimenopause Transitions and Concerns
- Menopause
- Menopause
- Menopause Checklist Podcast: Episode 1: A Wee Problem
- Menopause Checklist Podcast: Episode 6: Hello Lubricant!
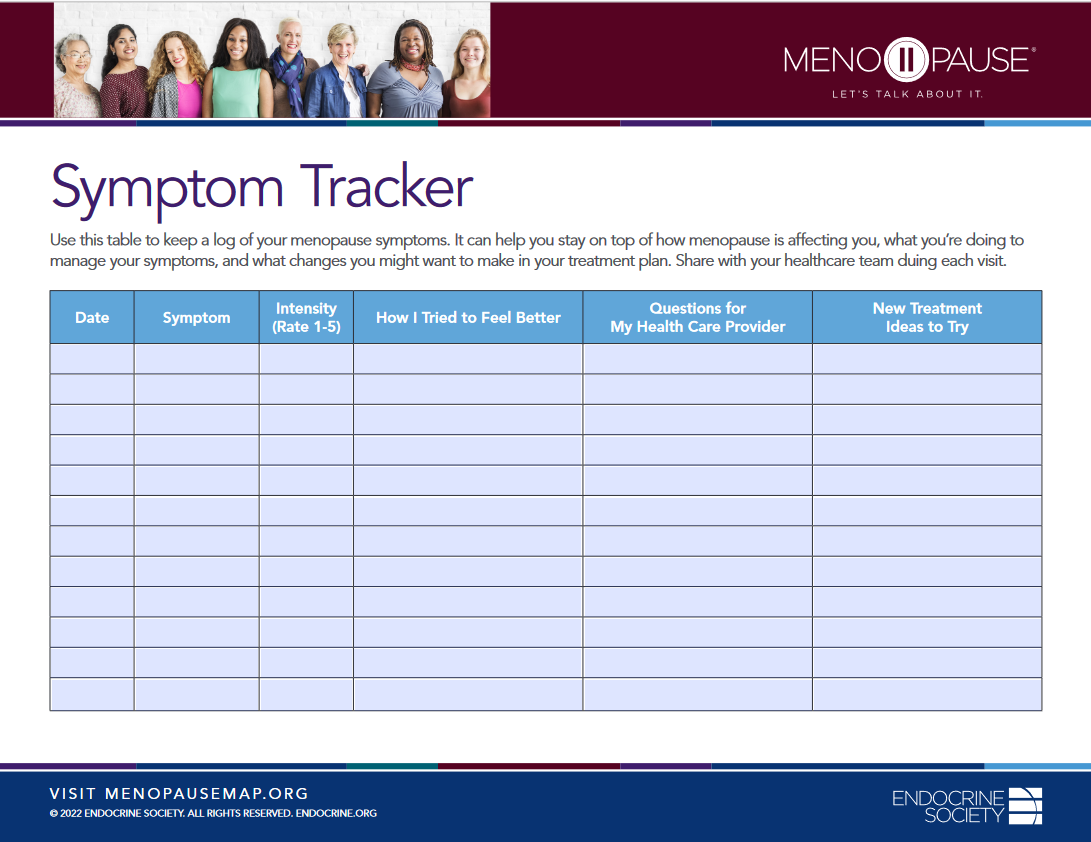
- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Questions for Your Health Care Provider
- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Symptom Tracker
- Menopause Patient Information [Videos] 2. Talking To Your GP About Menopause
- Menopause Ruining Your Sex Life?
- Menopause: Identification and Management [NICE Guideline Published: 12 November 2015 Last Updated: 07 November 2024]

- Menopause: Identification and Management: NICE Guideline [NG23] Published: 12 November 2015 Last Updated: 07 November 2024
- Navigating Menopause Together: How Partners Can Help
- Navigating Menopause: Honest Answers To All Your Questions [+ Video: What To Expect in Menopause]
- Navigating Menopause Care Resource Guide
- New AUA Guideline Offers Clinicians A Practical Toolbox for GSM Management [American Urological Association]
- Non-Hormonal Treatments Offer Relief for Genitourinary Syndrome of Menopause
- Painful Vaginal Sex (Dyspareunia)
- Pelvic Floor Health | Dr Louise Newson LIVE
- Perimenopause

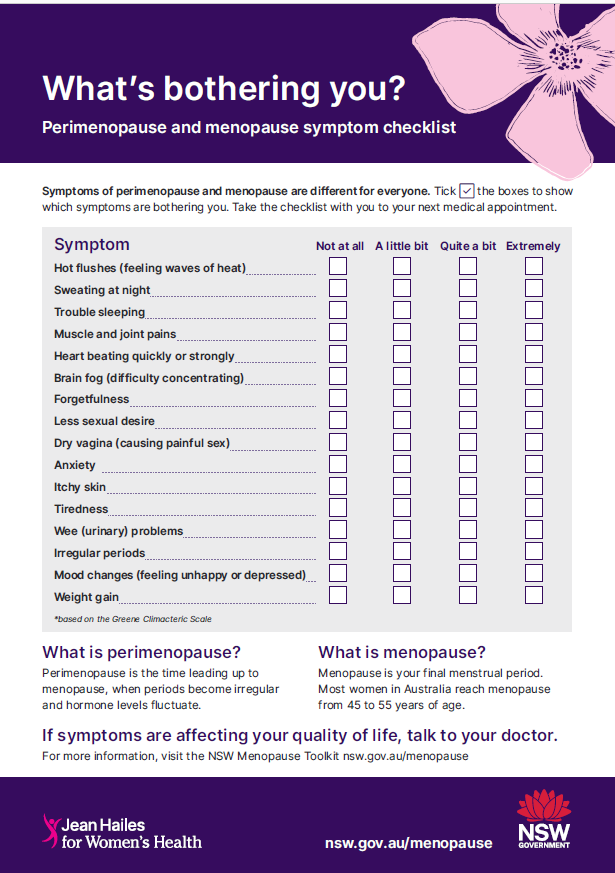
- Perimenopause and Menopause Symptom Checklist
- Preventing Urinary Tract Infections After Menopause: What Every Woman Should Know
- Questions To Ask Your GP About Menopause
- Struggling With UTIs After Menopause? Experts Say This Can Make A Difference
- Surprising Menopause Symptoms Q&A | Dr Louise Newson
- Symptoms of Menopause: Bladder, Vaginal and Vulval Problems
- The 2023 Practitioner’s Toolkit for Managing Menopause
- The Genitourinary Syndrome of Menopause: An Overview of the Recent Data
- The AUA/SUFU/AUGS Guideline on Genitourinary Syndrome of Menopause
- Therapeutic Choices for Genitourinary Syndrome of Menopause (GSM) In Breast Cancer Survivors: A Systematic Review and Update
- Topical Estrogens and Non-Hormonal Preparations for Postmenopausal Vulvovaginal Atrophy: An EMAS Clinical Guide
- Treating Incontinence During Your Perimenopause and Menopause Years
- Treatments for Menopause
- UTI: This Common Infection Can Be Serious
- Urinary Incontinence In Women
- Urogenital Problems
- Use of OTC Products and Persistent Vulvovaginal Irritation In Postmenopausal Women, With Caroline Mitchell, MD, MPH
- Vaginal Atrophy
- Vaginal Atrophy
- Vaginal Dryness
- Vaginal Dryness
- Vaginal Dryness
- Vaginal Dryness After Menopause: How To Treat It? I’m postmenopausal and often have vaginal dryness, which makes intercourse painful. Is there anything I can do about it?
- Vaginal Dryness: Alternative Treatments
- Vaginal Laser Therapy
- Videos & Podcasts: Videos – Genitourinary Syndrome of Menopause
- Videos & Podcasts: Videos – Menopause and Hormone Therapy: Current Perspectives and Controversies
- Vulval Irritation
- Webinars: The Burn, the Itch, the Pain, the Urge: GSM In Women
- What Is the Difference Between Vagifem and Estring?
- What Types of Vaginal Oestrogens Are There?
- Which Vaginal Moisturiser Should You Use?
- Why You Get An Itch or Thrush on Vaginal Estrogen and What To Do About It
- World Menopause Day 2024: Leaflet for Women – Menopause and Menopause Hormone Therapy [Multiply Languages]
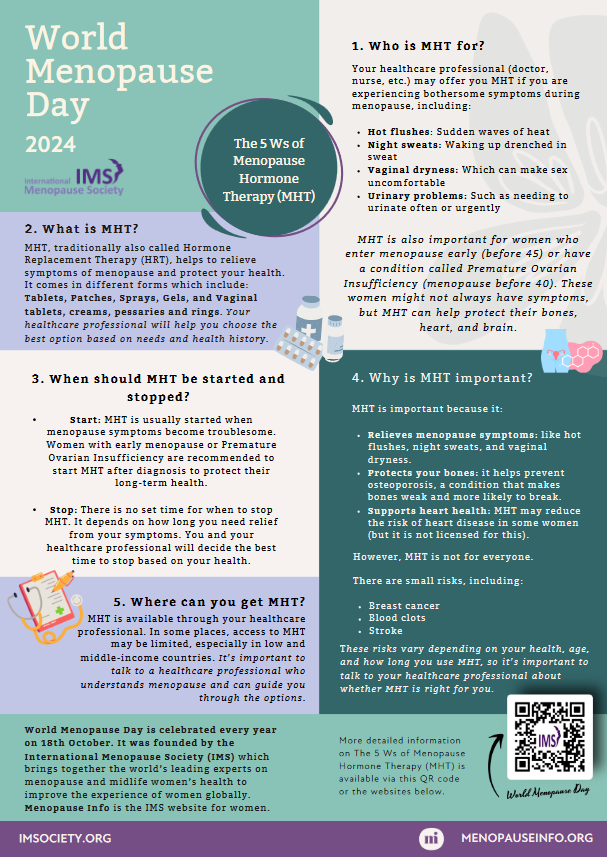 World Menopause Day 2024: Poster for Women – The 5 Ws of Menopause Hormone Therapy (MHT)
World Menopause Day 2024: Poster for Women – The 5 Ws of Menopause Hormone Therapy (MHT)
Sources
Where may I find the Sources quoted?
You may find the Sources quoted at:
Sources
- Genitourinary Syndrome of Menopause. 2025:1. Menopause Society https://menopause.org/wp-content/uploads/for-women/MenoNote-GSM.pdf Accessed: 14 January 2026
- Genitourinary Syndrome of Menopause. 2025:1. Menopause Society https://menopause.org/wp-content/uploads/for-women/MenoNote-GSM.pdf Accessed: 14 January 2026
- Vaginal Atrophy: Symptoms & Causes – Symptoms. 20 December 2025. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288 Accessed: 14 January 2026
- Symptoms of Menopause: Bladder, Vaginal and Vulval Problems. Last Updated: 15 October 2025. Last Reviewed: 23 April 2025. Jean Hailes for Women’s Health https://www.jeanhailes.org.au/health-a-z/menopause/menopause-symptoms/ Accessed: 14 January 2026
- Genitourinary Syndrome of Menopause: Key Points. 15 July 2024. Australasian Menopause Society https://www.menopause.org.au/hp/information-sheets/genitourinary-syndrome-of-menopause
- Vaginal Atrophy: Symptoms & Causes – Causes. 20 December 2025. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288 Accessed: 14 January 2026
- Genitourinary Syndrome of Menopause. 2025: 1-2. Menopause Society https://menopause.org/wp-content/uploads/for-women/MenoNote-GSM.pdf Accessed: 14 January 2026
- Genitourinary Syndrome of Menopause (GSM). Reviewed November 2025:1. British Menopause Society https://thebms.org.uk/wp-content/uploads/2025/11/09-NEW-BMS-ConsensusStatement-Genitourinary-Syndrome-of-Menopause-GSM-NOV2025-B.pdf Accessed: 14 January 2026
- Vaginal Atrophy: Symptoms & Causes – Symptoms: When To See A Doctor. 20 December 2025. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288 Accessed: 14 January 2026
- Deciding About Hormone Therapy Use. 2025:1. Menopause Society https://menopause.org/wp-content/uploads/default-document-library/MenoNote-Deciding-About-HT-2025.pdf Accessed: 14 January 2026
- Vaginal Atrophy: Symptoms & Causes – Prevention. 20 December 2025. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288 Accessed: 14 January 2026
- Genitourinary Syndrome of Menopause: AUA/SUFU/AUGS Guideline (2025). April 2025. American Urological Association https://www.auanet.org/guidelines-and-quality/guidelines/genitourinary-syndrome-of-menopause Accessed: 14 January 2026
- Davis, S. R., Taylor, S., Hemachandra, C., Magraith, K., Ebeling, P. R., Jane, F., and Islam12 September 2024, R. M. The 2023 Practitioner’s Toolkit for Managing Menopause: The 2023 Practitioner’s Toolkit for Managing the Menopause Supporting Notes – Effectiveness: Local Treatment of Urogenital Atrophy. Published Online: 30 October 2023 https://www.tandfonline.com/doi/full/10.1080/13697137.2023.2258783 Accessed: 14 January 2026
- Symptoms of Menopause: Bladder, Vaginal and Vulval Problems – Urinary Symptoms. Last Updated: 15 October 2025. Last Reviewed: 23 April 2025. Jean Hailes for Women’s Health https://www.jeanhailes.org.au/health-a-z/menopause/menopause-symptoms/ Accessed: 14 January 2026







