“Genitourinary syndrome of menopause is caused by
a decrease in estrogen production. Less estrogen
makes your vaginal tissues thinner, drier, less elastic…”.1
Umbrella
What may the Genitourinary Syndrome of Menopause Umbrella include?
Depending on the Source (DotS) this Umbrella may include:
- Atrophic Vaginitis
- Genital Atrophy
- Genitourinary/Genito-Urinary Syndrome of Menopause (GSM)
- Menopause Vaginal Dryness
- Urogenital Problems
- Vaginal Atrophy
- Vaginal Dryness
- Vaginal Symptoms
- Vulvovaginal Atrophy (VVA)
Definition
What is the genitourinary syndrome of menopause (GSM)?
DotS the definition of GSM may vary. On page one in Vaginal Dryness the North American Menopause Society (NAMS) elaborate on:
In Mayo Clinic Q and A: Treatment for Vaginal Dryness for Menopausal Women the (United States) Mayo Clinic elaborate on:
“Vaginal dryness is common in women who are approaching menopause and those who have gone through menopause. Other related symptoms include vaginal and vulvar irritation; burning or itching; discomfort or pain with sexual activity; and urinary symptoms, such as more frequent or urgent urination, urge leak, and urinary tract infections. Together, these symptoms are referred to as “genitourinary syndrome of menopause,” or GSM. These symptoms occur in roughly half of menopausal women and are even more common in women with breast cancer”.3
Common or Not
How common is GSM in postmenopausal women?
In Symptoms of Menopause: Bladder, Vaginal and Vulval Problems the (Australian) Jean Hailes for Women’s Health (JH) explain:
Symptoms
What may be symptoms of GSM?
In Vaginal Atrophy: Symptoms & Causes – Symptoms the Mayo Clinic explain:
- Vaginal dryness
- Vaginal burning
- Vaginal discharge
- Genital itching
- Burning with urination
- Urgency with urination
- Frequent urination
- Recurrent urinary tract infections
- Urinary incontinence
- Light bleeding after intercourse
- Discomfort with intercourse
- Decreased vaginal lubrication during sexual activity
- Shortening and tightening of the vaginal canal”.5
Cause
What causes GSM?
In Vaginal Atrophy: Symptoms & Causes – Causes the Mayo Clinic elaborate on:
“Genitourinary syndrome of menopause is caused by a decrease in estrogen production. Less estrogen makes your vaginal tissues thinner, drier, less elastic and more fragile”.6
Treatment
What are some GSM treatments?
On page one and two in Vaginal Dryness: Treatment Options the NAMS elaborate on:
 “There are many effective treatment options for GSM, including over-the-counter and prescription therapies. First-line therapies for less severe symptoms include nonhormone over-the-counter lubricants used as needed for sexual activity and moisturizers used regularly (several times per week) to maintain moisture. Prescription therapies include low-dose vaginal estrogens, vaginal dehydroepiandrosterone inserts, and oral ospemifene. Nonhormone lubricants and moisturizers can be combined for optimal symptom relief and can be used in combination with prescription therapies for more severe symptoms.
“There are many effective treatment options for GSM, including over-the-counter and prescription therapies. First-line therapies for less severe symptoms include nonhormone over-the-counter lubricants used as needed for sexual activity and moisturizers used regularly (several times per week) to maintain moisture. Prescription therapies include low-dose vaginal estrogens, vaginal dehydroepiandrosterone inserts, and oral ospemifene. Nonhormone lubricants and moisturizers can be combined for optimal symptom relief and can be used in combination with prescription therapies for more severe symptoms.
- “Nonhormone Remedies
- Vaginal Lubricants…
- Vaginal Moisturizers…
- Regular Sexual Stimulation…
- Expanding Your Views of Sexual Pleasure…
- Vaginal Dilators…
- Pelvic Floor Exercises…
- Vaginal Hormone Therapy…
- An effective and safe treatment, low-dose local estrogen applied directly to the vagina…
- FDA-approved low-dose vaginal estrogen products…
- Dehydroepiandrosterone (DHEA; Prasterone)
- Low-dose vaginal estrogen or DHEA may be options for women with a history breast or uterine cancer…
- Systemic Estrogen Therapy
- Other Therapies…
- Ospemifene
- Vaginal Laser Therapy…”.7
Painful Intercourse
How may painful intercourse be resolved?
The Mayo Clinic explain:
Vaginal Estrogen
How may vaginal estrogen be used?
In The 2022 Hormone Therapy Position Statement of The North American Menopause Society: Abstract published July 2022, the NAMS note:
“For bothersome genitourinary syndrome of menopause symptoms not relieved with over-the-counter therapies in women without indications for use of systemic hormone therapy, low-dose vaginal estrogen therapy or other therapies (eg, vaginal dehydroepiandrosterone or oral ospemifene) are recommended”.9
Can estrogen be placed directly into the vagina?
On page one in Deciding About Hormone Therapy Use, published July 2022, the NAMS explain:
“If you are bothered only by vaginal dryness, you can use very low doses of estrogen placed directly into the vagina. These low doses generally do not raise blood estrogen levels above postmenopause levels and do not treat hot flashes. You do not need to take a progestogen when using only low doses of estrogen in the vagina. (The MenoNote “Vaginal Dryness” covers this topic in detail)”.10
On page three in the Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause, first published online 10 June 2022, one of the recommendations is:
- “Low-dose and ultra-low dose vaginal oestrogen preparations can be taken by perimenopausal and menopausal women experiencing genitourinary symptoms and continued for as long as required. All vaginal oestrogen preparations have been shown to be effective in this context and there is no requirement to combine vaginal oestrogens with systemic progestogen treatment for endometrial protection, as low-dose and ultra-low dose vaginal oestrogen preparations do not result in significant systemic absorption or endometrial hyperplasia”.11
Health Care Provider
What if I think I have GSM?
If you think you have GSM, it may be in your best interest to choose to talk to your health care provider about this.
In The 2023 Practitioner’s Toolkit for Managing Menopause – Effectiveness: Local Treatment of Urogenital Atrophy, published online 01 December 2023, the authors note:
In Symptoms of Menopause: Bladder, Vaginal and Vulval Problems – Urinary Symptoms the JH explain:
On page two in Vaginal Dryness the NAMS also note:
Health Topics A-Z
Where may I find Health Topics A-Z related to Genitourinary Syndrome of Menopause?
In Health Topics A-Z you may find:
Links
Where may I find Links related to Genitourinary Syndrome of Menopause?
Your Country may have Links similar to:
Links
This Links List to third party websites is neither comprehensive nor exhaustive. Inclusion on this Links List does not imply endorsement or recommendation. Non-inclusion on this Links List does not imply non-endorsement or non-recommendation. Third party websites are not under the control of Meno Martha International Menopause Directory. Third party websites may contain explicit medical images and/or sexual references. Please read Meno Martha International Menopause Directory’s Links Policy before proceeding to a Link. Please contact Webmaster if you experience a problem with a Link.New or Updated
- Genitourinary Syndrome of Menopause (Vaginal Atrophy)
- Genitourinary Syndrome of Menopause [Podcast]
- Genitourinary Syndrome of Menopause: New Name, Old Problem
- Is it too late to start HRT? [15 July 2024]
- Prof. J. Shifren – Genitourinary Syndrome of Menopause | Consumer
- Video Series-2024: Preparing for Your Menopause Health Care Visit [13 January 2024]
- ACOG Explains: Managing Menopause Symptoms [American College of Obstetricians and Gynecologists]
- Askearlymenopause.org [+ Video: What Is Early Menopause?]
- BMS TV: Urogenital Atrophy
- Bioidentical Hormones: Are They Safer?
- Bladder Control: Lifestyle Strategies Ease Problems
- CO2-Laser Therapy and Genitourinary Syndrome of Menopause: A Systematic Review and Meta-Analysis
- Caredownthere .org [Care Down There, Australia]
- Deciding About Hormone Therapy Use
- Douching Fact Sheet
- Dr. Stephanie Faubion – Genitourinary Syndrome of Menopause
- Endometrial Safety of Low-Dose Vaginal Estrogens
- Endometrial Safety of Low-Dose Vaginal Estrogens [Video]
- Experiencing Vaginal Dryness? Here’s What You Need To Know
- Find A Menopause Practitioner [United States and Other]
- Find An AMS Doctor [Australasian Menopause Society i.e. Australia and New Zealand]
- Find Your Nearest BMS Menopause Specialist [British Menopause Society]
- Genitourinary Syndrome of Menopause (GSM)
- Genitourinary Syndrome of Menopause (Vaginal Atrophy)
- Genitourinary Syndrome of Menopause [Podcast]
- Genitourinary Syndrome of Menopause and the False Promise of Vaginal Laser Therapy
- Genitourinary Syndrome of Menopause: A Systematic Review on Prevalence and Treatment [Video]
- Genitourinary Syndrome of Menopause: New Name, Old Problem
- Hormone Therapy: Is It Right for You?
- Hormone Replacement Therapy (HRT): Vaginal Oestrogen – Common Questions About Vaginal Oestrogen
- Hormone Replacement Therapy (HRT): Vaginal Oestrogen – How and When To Use Vaginal Oestrogen
- International Society for the Study of Women’s Sexual Health: Find A Provider
- Is it too late to start HRT?
- Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause
- Laser Treatment for Genitourinary Syndrome of Menopause (Scientific Impact Paper No. 72)
- Later Years (Around 50 Years and Over): Menopause and Post Menopause Health – Sexual Wellbeing, Intimacy and Menopause [+ Video: Menopause Is the End of Your Sex Life]
- Low Estrogen Bladder Symptoms and Treatment
- Lubricant Alternatives: What To Use and What To Avoid
- Mayo Clinic Minute: Menopause and Sexual Health [+ Video Courtesy: Mayo Clinic News Network]
 Mayo Clinic Q and A: 6 UTI Myths and Facts
Mayo Clinic Q and A: 6 UTI Myths and Facts- Mayo Clinic Q and A: Perimenopause Transitions and Concerns
- Menopause
- Menopause
- Menopause Checklist Podcast: Episode 1: A Wee Problem
- Menopause Management Options
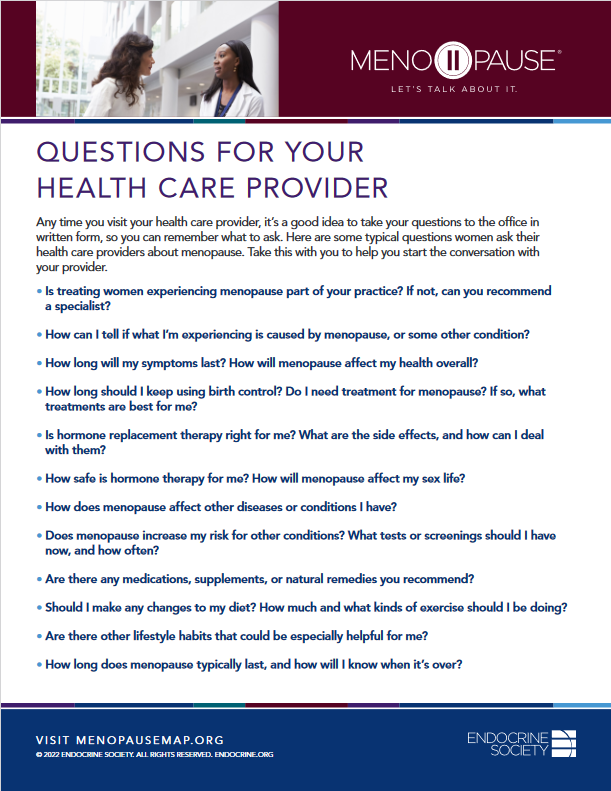
- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Questions for Your Health Care Provider
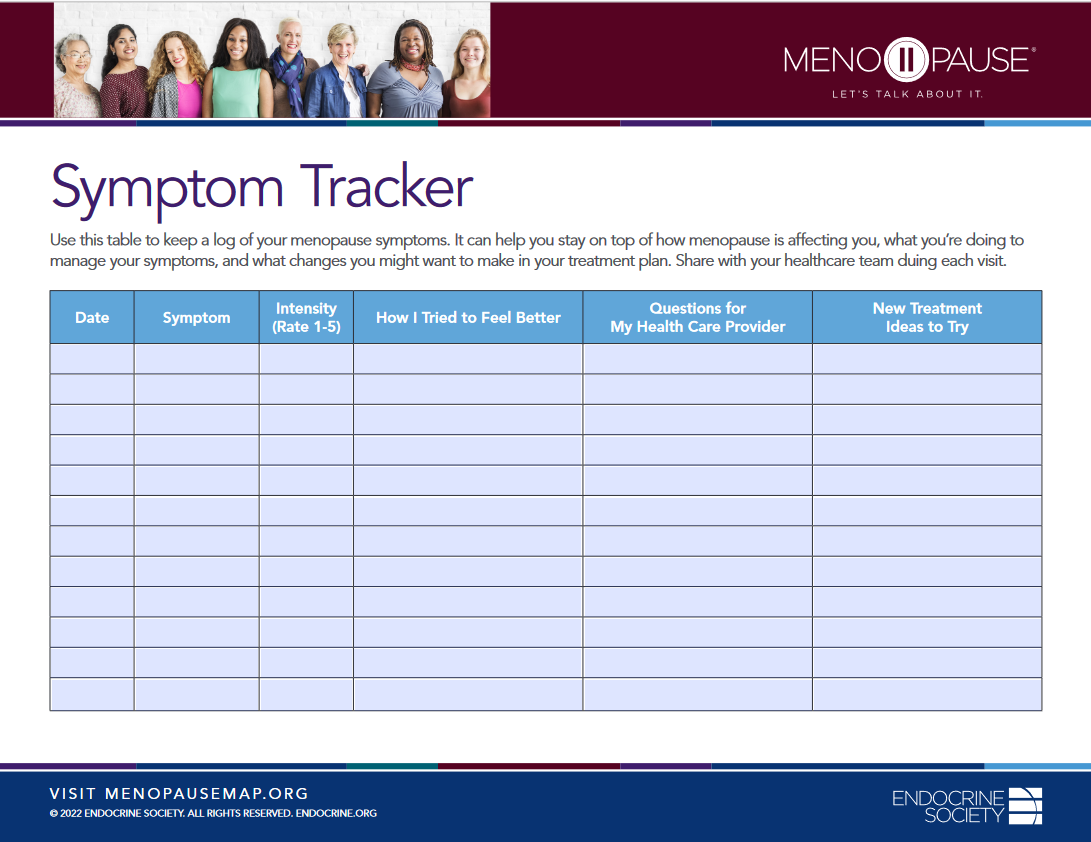
- Menopause Map: Downloadable Resources – My Personal Path Print Tools: Symptom Tracker
- Menopause Patient Information [Videos] 2. Talking To Your GP About Menopause
- Menopause Preparedness Toolkit Video Series: Common Conditions Associated With Menopause and Midlife
- Menopause Preparedness Toolkit Video Series: Lifestyle Tips for Menopause Wellness
 Menopause Preparedness Toolkit: A Woman’s Empowerment Guide
Menopause Preparedness Toolkit: A Woman’s Empowerment Guide- Menopause Ruining Your Sex Life?
- Menopause Symptoms: Mayo Clinic Expert Outlines Hormone and Nonhormonal Therapies
- Menopause Treatments: What Works, What Doesn’t
- Menopause, Perimenopause, Hormone Therapy and Other Treatments With Madelyn Butler, MD [Podcast]
- Menopause: Diagnosis and Management – Information for the Public: Questions To Ask About Menopause [NICE Guideline]
- Menopause: Understanding the Changes and Finding Relief | Dr Susan Davis | The Proof Podcast EP 256
- Mymenoplan.org [My Menoplan, United States]
- Navigating Menopause Together: How Partners Can Help
- Navigating Menopause: Expert Insights and Solutions | Dr Susan Davis | The Proof Podcast EP 245
- Navigating Menopause: Honest Answers To All Your Questions [+ Video: What To Expect in Menopause]
- Painful Vaginal Sex (Dyspareunia)
- Patty Brisben Foundation for Women’s Sexual Health: Guide To Sexual Health Providers
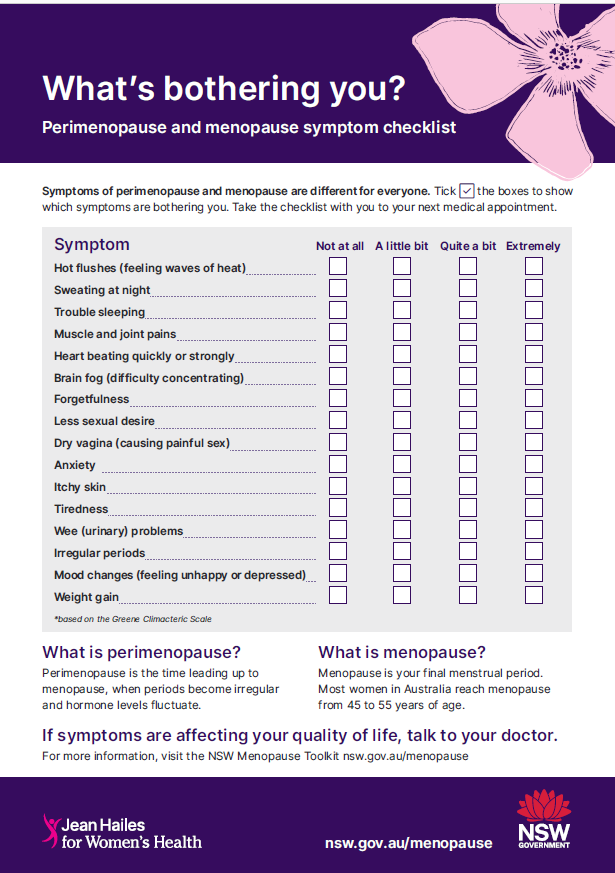
- Perimenopause and Menopause Symptom Checklist
- Position Statement for Management of Genitourinary Syndrome of the Menopause (GSM)
- Prof. J. Shifren – Genitourinary Syndrome of Menopause | Consumer
- Prosayla Supported By ISSWSH [International Society for the Study of Women’s Sexual Health]
- Questions To Ask Your GP About Menopause
- Sexual Difficulties In the Menopause
- Symptoms of Menopause: Bladder, Vaginal and Vulval Problems
- The 2020 Genitourinary Syndrome of Menopause Position Statement of The North American Menopause Society
- The 2023 Practitioner’s Toolkit for Managing Menopause
- The Genitourinary Syndrome of Menopause: An Overview of the Recent Data
- The Vaginal Laser Therapy Versus Vaginal Estrogen Therapy: The VeLVET Trial [Video]
- Tips To Help Manage Menopause Symptoms
- Therapeutic Choices for Genitourinary Syndrome of Menopause (GSM) In Breast Cancer Survivors: A Systematic Review and Update
- The Truth About Menopause Supplements | Dr Sarah Berry
- Therapy for the Effects of Menopause
- Tips To Help Manage Menopause Symptoms
- Treating Genitourinary Syndrome of Menopause In Breast Cancer Survivors
- Treating Incontinence During Your Perimenopause and Menopause Years
- UTI: This Common Infection Can Be Serious
- Urogenital Problems
- Urologic View In the Management of Genitourinary Syndrome of Menopause
- Using Natural Therapies In the Menopause Transition – Webinar
- Vaginal Atrophy
- Vaginal Atrophy
- Vaginal Dryness
- Vaginal Dryness
- Vaginal Dryness
- Vaginal Dryness After Menopause: How To Treat It? I’m postmenopausal and often have vaginal dryness, which makes intercourse painful. Is there anything I can do about it?
- Vaginal Dryness: Alternative Treatments
- Vaginal Dryness: What To Do About It
- Vaginal Laser Therapy for GSM/VVA: Where We Stand Now – A Review By the EUGA Working Group on Laser
- Vaginal Laser Therapy for Genitourinary Syndrome of Menopause – Systematic Review
- Video & Podcast Library: Interviews – Video: Genitourinary Syndrome of Menopause
- Video Series-2023: NAMS 2023 Nonhormone Therapies Position Statement for Bothersome Menopause Symptoms
- Video Series-2023: Premature and Early Menopause
- Video Series-2024: Preparing for Your Menopause Health Care Visit
- Videos and Podcasts: Videos – Interviews: A Simple Approach To Menopause: The Menopause Quick Six (www.MQ6.ca)
- Vulval Irritation
- Vulvovaginal Atrophy
- Webinars: Previous – Non-Pharmacological Interventions For VMS
- Webinars: Previous – Pay Attention on Your Way In! The Vulva Is An Important Organ Too
- What Everyone Should Know About Menopause Symptoms
- Why Didn’t Anyone Tell Me This? Episode 3: Dr Annice Mukherjee: Your Essential Menopause Toolkit
Sources
Where may I find the Sources quoted?
You may find the Sources quoted at:
Sources
- Vaginal Atrophy: Symptoms & Causes – Causes. 17 September 2021. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288 Accessed: 19 April 2024
- Vaginal Dryness. 2022: 1. North American Menopause Society https://www.menopause.org/docs/default-source/for-women/mn-vaginal-dryness.pdf Accessed: 19 April 2024
- Mayo Clinic Q and A: Treatment for Vaginal Dryness for Menopausal Women. 14 July 2021. Mayo Clinic https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-treatment-for-vaginal-dryness-for-menopausal-women/ Accessed: 19 April 2024
- Symptoms of Menopause: Bladder, Vaginal and Vulval Problems. Last Updated: 28 March 2024. Last Reviewed: 19 August 2022. Jean Hailes for Women’s Health https://www.jeanhailes.org.au/health-a-z/menopause/menopause-symptoms/ Accessed: 19 April 2024
- Vaginal Atrophy: Symptoms & Causes – Symptoms. 17 September 2021. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288 Accessed: 19 April 2024
- Vaginal Atrophy: Symptoms & Causes – Causes. 17 September 2021. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288 Accessed: 19 April 2024
- Vaginal Dryness: Treatment Options. 2022: 1-2. North American Menopause Society https://www.menopause.org/docs/default-source/for-women/mn-vaginal-dryness.pdf Accessed: 19 April 2024
- Vaginal Atrophy: Symptoms & Causes – Symptoms: When To See A Doctor. 17 September 2021. Mayo Clinic https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288 Accessed: 19 April 2024
- The 2022 Hormone Therapy Position Statement of The North American Menopause Society: Abstract. Published July 2022. The North American Menopause Society https://journals.lww.com/menopausejournal/Abstract/2022/07000/The_2022_hormone_therapy_position_statement_of_The.4.aspx Accessed: 05 December 2023
- Deciding About Hormone Therapy Use. Published July 2022. The North American Menopause Society https://www.menopause.org/docs/default-source/professional/menonote-deciding-about-ht-2022.pdf Accessed: 19 April 2024
- Hamoda, H., Mukherjee, A., Morris, E., Baldeweg, S. E., Jayesena, C. N., Briggs, P., Moger, S. Joint Position Statement By the British Menopause Society, Royal College of Obstetricians and Gynaecologists and Society for Endocrinology on Best Practice Recommendations for the Care of Women Experiencing the Menopause. First Published Online 10 June 2022 https://journals.sagepub.com/doi/full/10.1177/20533691221104879 Accessed: 19 April 2024
- Davis, S. R., Taylor, S., Hemachandra, C., Magraith, K., Ebeling, P. R., Jane, F., and Islam, R. M. The 2023 Practitioner’s Toolkit for Managing Menopause: The 2023 Practitioner’s Toolkit for Managing the Menopause Supporting Notes – Effectiveness: Local Treatment of Urogenital Atrophy. Published Online: 30 October 2023 https://www.tandfonline.com/doi/full/10.1080/13697137.2023.2258783 Accessed: 19 April 2024
- Symptoms of Menopause: Bladder, Vaginal and Vulval Problems – Urinary Symptoms. Last Updated: 28 November 2023. Last Reviewed: 19 August 2022. Jean Hailes for Women’s Health https://www.jeanhailes.org.au/health-a-z/menopause/menopause-symptoms/ Accessed: 19 April 2024
- Vaginal Dryness: Note. 2022: 2. North American Menopause Society https://www.menopause.org/docs/default-source/for-women/mn-vaginal-dryness.pdf Accessed: 19 April 2024



