“It is best to let your vagina clean itself. The vagina
cleans itself naturally by making mucous. The mucous
washes away blood, semen, and vaginal discharge”.1
Umbrella
What may the Vaginal and Vulval Hygiene Umbrella include?
Depending on the Source (DotS) this Umbrella may include:
- Genital Care/Health/Hygiene
- Vaginal Care/Health/Hygiene
- Vulval Care/Health/Hygiene
Self-Cleaning
Is the vagina self-cleaning?
In Douching: What Is the Best Way To Clean My Vagina? the Office on Women’s Health, United States Department of Health and Human Services, Womenshealth.gov elaborate on:
“It is best to let your vagina clean itself. The vagina cleans itself naturally by making mucous. The mucous washes away blood, semen, and vaginal discharge”.2
Douching
What is douching?
DotS the definition of douching may vary. In Feminine Odor Problems? What Every Woman Needs To Know the (United States) Cleveland Clinic’s definition is:
In Douching: What Is Douching? Womenshealth.gov’s definition is:
“The word “douche” means to wash or soak. Douching is washing or cleaning out the inside of the vagina with water or other mixtures of fluids. Most douches are sold in stores as prepackaged mixes of water and vinegar, baking soda, or iodine. The mixtures usually come in a bottle or bag. You squirt the douche upward through a tube or nozzle into your vagina. The water mixture then comes back out through your vagina”.4
Bath/Shower
Is douching different from washing the outside of your vagina during a bath or shower?
In Douching: What Is Douching? Womenshealth.gov’s explain:
Why Not
Why should women not douche?
In Douching: Why Should Women Not Douche? the Womenshealth.gov elaborate on:
A healthy vagina has good and harmful bacteria. The balance of bacteria helps maintain an acidic environment. The acidic environment protects the vagina from infections or irritation.
Douching can cause an overgrowth of harmful bacteria. This can lead to a yeast infection or bacterial vaginosis. If you already have a vaginal infection, douching can push the bacteria causing the infection up into the uterus, fallopian tubes, and ovaries. This can lead to pelvic inflammatory disease, a serious health problem.
Douching is also linked to other health problems”.6
Keeping Clean
How may women keep their vagina clean?
In Essential Information: Caring for Your Skin Down There – Cleansing the (Australian) Caredownthere elaborate on:
 “Just in case you have been wondering if your vulval problem is happening because you aren’t washing enough….you don’t have a hygiene problem. Using soap, particularly if this is done frequently, will in fact make your skin more sensitive. It is best to avoid soap, particularly perfumed liquid soaps, abrasive washes and wet wipes. A soap substitute, available from your chemist, or simply soaking in a bath with a couple of handfuls of ordinary salt thrown in is the best way to clean vulval skin”.7
“Just in case you have been wondering if your vulval problem is happening because you aren’t washing enough….you don’t have a hygiene problem. Using soap, particularly if this is done frequently, will in fact make your skin more sensitive. It is best to avoid soap, particularly perfumed liquid soaps, abrasive washes and wet wipes. A soap substitute, available from your chemist, or simply soaking in a bath with a couple of handfuls of ordinary salt thrown in is the best way to clean vulval skin”.7
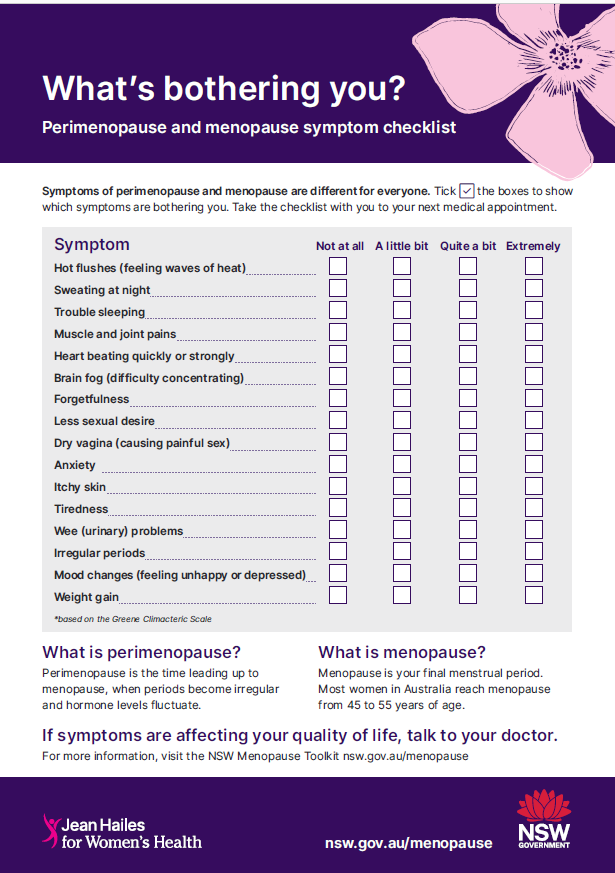
Postmenopause Odour
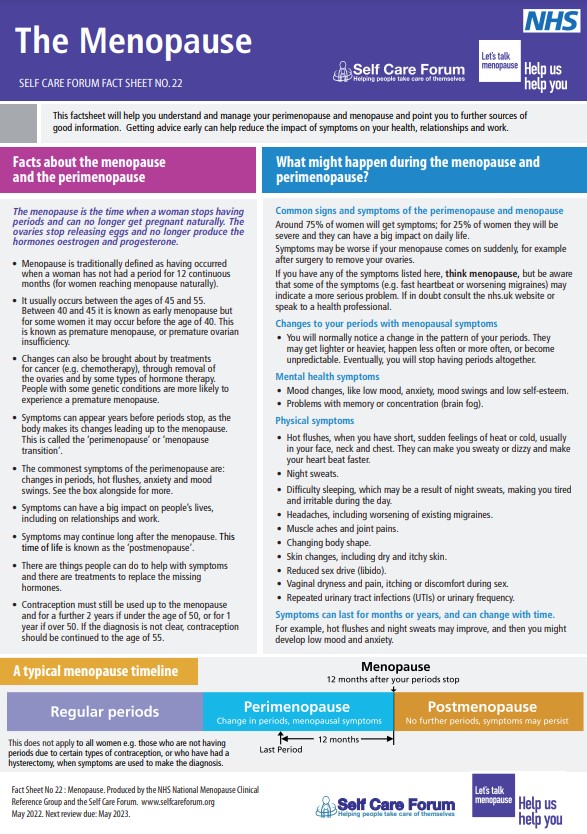
Postmenopause or after menopause, may vaginal smell change?
In Vulva and Vagina: What’s Normal? Smell [+ Image] the (Australian) Jean Hailes for Women’s Health (JH) elaborate on:
“After menopause, the smell may be different to when you were having periods because the bacteria in your vagina changes at this time”.8
In Feminine Odor Problems? What Every Woman Needs To Know the Cleveland Clinic explain:
Health Care Provider
What if I am worried about what is going on down there?
If you are worried about what is going on down there, it may be in your best interest to choose to talk to your health care provider about this. The JH note:
“If you are worried about the smell, or have symptoms such as itching, burning, irritation, soreness, painful sex or pain when you wee, see your doctor”.10
In Vagina: What’s Typical, What’s Not – What Are Signs or Symptoms of Vaginal Problems? the (United States) Mayo Clinic explain:
- A change in the color, odor or amount of vaginal discharge
- Vaginal redness or itching
- Vaginal bleeding between periods, after sex or after menopause
- A mass or bulge in the vagina
- Pain during intercourse”.11
Health Topics A-Z
Where may I find Health Topics A-Z related to the Vaginal and Vulval Hygiene?
In Health Topics A-Z you may find:
Links
Where may I find Links related to Vaginal and Vulval Hygiene?
Your Country may have Links similar to:
Links
This Links List to third party websites is neither comprehensive nor exhaustive. Inclusion on this Links List does not imply endorsement or recommendation. Non-inclusion on this Links List does not imply non-endorsement or non-recommendation. Third party websites are not under the control of Meno Martha International Menopause Directory. Third party websites may contain explicit medical images and/or sexual references. Please read Meno Martha International Menopause Directory’s Links Policy before proceeding to a Link. Please contact Webmaster if you experience a problem with a Link.New or Updated
- Q&A: Normalize Seeking Proper Bacterial Vaginosis Diagnosis, Treatment [08 March 2024]
- Sexual Problems and Menopause
- Vulva and Vagina
- Vulval and Vaginal Conditions
- Vulval Irritation: What You can Do To Look After Your Vulva [+ Video]
- Webinars: Previous – Pay Attention on Your Way In! The Vulva Is An Important Organ Too
- 10 Embarrassing Questions You Should Ask Your Doctor
- 5 Common Problems ‘Down There’ — and Whether They Are Contagious
- 9 Tips To Keep Your Vagina and Vulva Healthy
- Are Probiotics Good for Vaginal Health?
- BMS TV: Urogenital Atrophy
- Bacterial Vaginosis
- Bacterial Vaginosis
- Caredownthere.com.au
- Douching
- Essential Information: Caring for Your Skin Down There
- FAQs: Disorders of the Vulva: Common Causes of Vulvar Pain, Burning, and Itching
- FAQs: Vulvovaginal Health
- Feminine Odor Problems? What You Should Know About Douching
- Hormonal Health – Clues Made Clear
- International Society for Sexual Medicine: Public
- International Society for Sexual Medicine: Sexual Health Topics
- International Society for the Study of Vulvovaginal Disease
- International Society for the Study of Vulvovaginal Disease: Patient Handouts
- International Society for the Study of Women’s Sexual Health
- International Society for the Study of Women’s Sexual Health: Find A Provider
- Lichen Planus
- Lichen Planus
- Lichen Sclerosus
- Lichen Sclerosus
- Menopause Management: Managing Vaginal Problems
- Menopause Patient Information: 2. Talking To Your GP About Menopause
- Menopause Preparedness Toolkit Video Series: Common Conditions Associated With Menopause and Midlife
- National Center for Complementary and Integrative Health: How Safe Is This Product or Practice?
- National Center for Complementary and Integrative Health: Natural Doesn’t Necessarily Mean Safer, or Better
- Patty Brisben Foundation for Women’s Sexual Health
- Patty Brisben Foundation for Women’s Sexual Health: Guide To Sexual Health Providers
- Patty Brisben Foundation for Women’s Sexual Health: New! Sexual Anatomy 101
- Prosayla Supported by ISSWSH [International Society for the Study of Women’s Sexual Health]
- Q&A: Normalize Seeking Proper Bacterial Vaginosis Diagnosis, Treatment
- Self-Help Tips
- Sexual Problems and Menopause
- The Vulva: Irritation, Diagnosis & treatment – Booklet
- Tips To Help Manage Menopause Symptoms
- Top Tips for Talking To Your Doctor
- Urogenital Problems
- Vagina: What’s Typical, What’s Not
- Vaginal Candiasis
- Vaginal Discharge
- Vaginal Discharge
- Vaginal Discharge
- Vaginal Dryness
- Vaginal Dryness
- Vaginal Dryness: What To Do About It
- Vaginal Pain
- Video Series-2022: Discussing Sexual Health Concerns With Your Health Care Professional
- Video Series-2022: Perimenopause, Signs, Symptoms, and Solutions
- Video Series-2023: Changes In Sexual Health After Cancer
- Vulva and Vagina
- Vulval Irritation
- Vulval and Vaginal Conditions
- Vulvar Awareness Day [18 September 2023]
- Vulvovaginal Thrush
- Webinars: Previous – Pay Attention on Your Way In! The Vulva Is An Important Organ Too
- Webinars: Previous – Sexual Health Issues In Menopause
- What Is Vaginal Steaming and Is It Safe?
- Why You Should Never Douche
- Yeast Infection (Vaginal)
Sources
Where may I find the Sources quoted?
You may find the Sources quoted:
Sources
- Douching: What Is the Best Way To Clean My Vagina? Page Last Updated: 29 December 2022. Office on Women’s Health, United States Department of Health and Human Services, Womenshealth.gov https://www.womenshealth.gov/a-z-topics/douching Accessed: 04 April 2024
- Douching: What Is the Best Way To Clean My Vagina? Page Last Updated: 29 December 2022. Office on Women’s Health, United States Department of Health and Human Services, Womenshealth.gov https://www.womenshealth.gov/a-z-topics/douching Accessed: 04 April 2024
- Feminine Odor Problems? What Every Woman Needs To Know. 10 June 2021. Cleveland Clinic https://health.clevelandclinic.org/feminine-odor-problems-what-you-should-know-about-douching/ Accessed: 04 April 2024
- Douching: What Is Douching? Page Last Updated: 29 December 2022. Office on Women’s Health, United States Department of Health and Human Services, Womenshealth.gov https://www.womenshealth.gov/a-z-topics/douching Accessed: 04 April 2024
- Douching: What Is Douching? Page Last Updated: 29 December 2022. Office on Women’s Health, United States Department of Health and Human Services, Womenshealth.gov https://www.womenshealth.gov/a-z-topics/douching Accessed: 04 April 2024
- Douching: Why Should Women Not Douche? Page Last Updated: 29 December 2022. Office on Women’s Health, United States Department of Health and Human Services, Womenshealth.gov https://www.womenshealth.gov/a-z-topics/douching Accessed: 04 April 2024
- Essential Information: Caring for Your Skin Down There – Cleansing. Caredownthere https://www.caredownthere.com.au/_pages/information_care.html Accessed: 04 April 2024
- Vulva and Vagina: What’s Normal? Smell. Last Updated: 07 December 2023 | Last Reviewed: 26 April 2023. https://www.jeanhailes.org.au/health-a-z/vulva-vagina/vulva-and-vagina#whats-normal Accessed: 04 April 2024
- Feminine Odor Problems? What Every Woman Needs To Know. 10 June 2021. Cleveland Clinic https://health.clevelandclinic.org/feminine-odor-problems-what-you-should-know-about-douching/ Accessed: 04 April 2024
- Vulva and Vagina: What’s Normal? Smell. Last Updated: 07 December 2023 | Last Reviewed: 26 April 2023. https://www.jeanhailes.org.au/health-a-z/vulva-vagina/vulva-and-vagina#whats-normal Accessed: 04 April 2024
- Vagina: What’s Typical, What’s Not – What Are Signs or Symptoms of Vaginal Problems? 06 December 2022. Mayo Clinic https://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/vagina/art-20046562 Accessed: 04 April 2024